In July of 2018, James Kypuros woke up to find his toes clenched and claw-like, as if fisted. “It was a little bit weird walking this way, because you didn't have that balance of your toes extended,” recalls the 76-year-old Cedar Lake, Indiana resident. That summer marked the beginning of a host of debilitating symptoms that would defy significant treatment response until James came to Mayo Clinic, where specialized testing diagnosed him with glycine receptor antibody syndrome. But that was still a ways ahead.
Shortly after his toes fisted, James started having falls. They happened at home and while at his job as a loan officer. For a time, he could get back up himself. Then one Saturday in August, while he and his wife were at their condo at Pine Lake, “I fell down in the garage and I couldn't get up,” says James. “My wife was with me, and she had to get some neighbors to help get me up. We went to the emergency room at University of Chicago Medical Center.” Unable to stand, James needed a wheelchair to be admitted. “Once they got me into a bed, I couldn’t sit up or even lift my feet off the bed. It was scary.”
Jim was initially diagnosed with stiff-person syndrome (SPS), a rare autoimmune disorder of the nervous system, often resulting in progressive, severe muscle stiffness and spasms of the lower extremities and back. Stiff-person syndrome affects about one in every million people. The disease has received more attention since 2022, when singer Celine Dion publicly revealed she suffers from SPS — which can be difficult to diagnose because it mimics other autoimmune disorders.

There was other bad news for James while in the hospital. He was diagnosed with the onset of chronic lymphocytic leukemia (CLL). After 17 days in Chicago Medical Center, James was transferred to Shirley Ryan AbilityLab in downtown Chicago. “When I got there, I could barely sit up by myself,” he recounts. “They took me from that to where I could walk with the aid of a walker.”
Amid his rehab, James also spent 10 days at Northwestern Memorial Hospital where his conditions of SPS and encephalomyopathy were reconfirmed. But doctors had yet to pinpoint a root cause behind his symptoms. Meanwhile, alarmed at how much he was suffering, James’s wife made an appointment for him at Mayo Clinic in Rochester, Minnesota. That gesture would change his life.
“We went to Mayo Clinic in November of ’18,” James says. “And that's when I met Dr. Flanagan.”
From rock bottom to dramatic healing
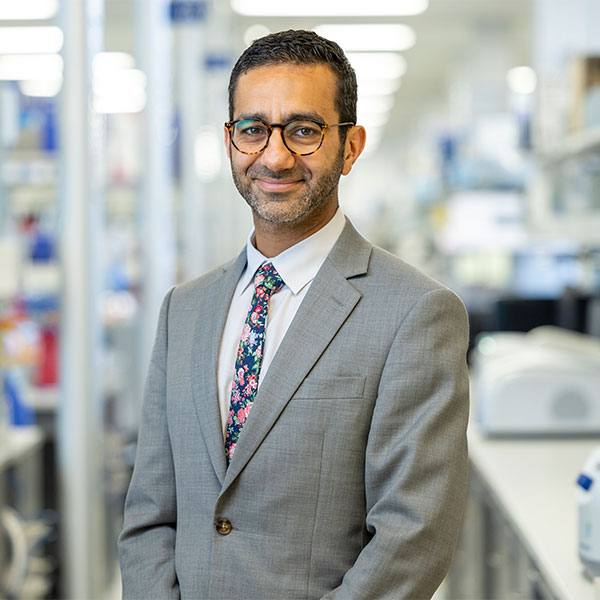
Eoin Flanagan, M.B., B.Ch., is a professor of neurology and chair of Mayo’s Division of Multiple Sclerosis and Autoimmune Neurology.
“WHEN JAMES CAME TO US, HE WAS STRUGGLING TO WALK,” SAYS DR. FLANAGAN. “HE ALSO REPORTED HAVING DOUBLE VISION AND DIFFICULTY SWALLOWING. SO WHEN WE SAW THAT ALONG WITH THE ENCEPHALOMYOPATHY, WE DECIDED TO RUN THE GLYCINE TEST, BECAUSE WE KNOW THAT GLYCINE RECEPTOR ANTIBODY SYNDROME CAN SOMETIMES BE ASSOCIATED WITH THOSE SYMPTOMS.”
The glycine receptor antibody was first discovered at Oxford University Hospitals in 2008. Mayo Clinic then developed a specialized test (Mayo ID: GLYCS) and currently is the only lab in the country to offer it. The assay demands a high level of expertise.

Andrew McKeon, M.B., B.Ch., M.D., a neurologist, professor of laboratory medicine and pathology, and director of the Neuroimmunology Laboratory at Mayo Clinic, explains what happens in glycine receptor antibody syndrome. “Glycine receptors are part of the inhibitory nervous system. You need glycine receptors to tone down the nervous system,” he says. “So you have this kind of yin and yang of excitation and inhibition in the nervous system that keeps things sort of on an even keel. And if your glycine receptors aren't functioning properly, you have way too much excitation, and then all the muscles become really stiff, and they start to spasm and can lock up. So what happens is that these antibodies, they bind to the glycine receptors, and then the receptors stop functioning.”
To bring home just how dangerous this syndrome can be, Dr. McKeon offers a comparison with strychnine poisoning. “With strychnine poisoning, the poison irreversibly binds to glycine receptors, and it produces a similar syndrome to PERM [a rarer form of stiff-person syndrome]. Except of course, with strychnine poisoning it’s way worse and immediately fatal. But the underlying commonality between the two is that it involves disruption of the glycine receptors.”
In December, James’s test results came back.
“THE GLYCINE RECEPTOR ANTIBODY WAS POSITIVE IN BOTH HIS BLOOD AND SPINAL FLUID, AND A KEY TO HIS DIAGNOSIS AND TREATMENT PLAN,” SAYS DR. FLANAGAN.
If not treated appropriately, stiff-person syndrome can have an associated mortality if the whole body “locks up,” because it can potentially disrupt a person’s breathing. Fortunately, James was in the right place for the right treatment. And because James also presented with CLL, Dr. Flanagan worked closely with Saad Kenderian, M.B., Ch.B., an oncologist and consultant in Mayo Clinic’s Division of Hematology.
For five days, James was put on a regiment of intravenous steroids, which then continued once a week for 11 weeks. The doctors then contacted James’s care team at Northwestern and recommended that he receive infusions of Rituxan, also known as rituximab, once he left Mayo. “He had a dramatic improvement with that treatment,” says Dr. Flanagan.
Jim wholeheartedly concurs, saying, “As soon as I did the five days of steroids, I could walk without any assistance. Dr. Flanagan is an incredible guy.”
For about two years, James’s life was mostly smooth sailing. Then, earlier this year, he had a month-long bout of severe nausea. “Some days I couldn't get out of bed,” he says. “The minute I tried to move, I felt like I was gonna lose everything. It was horrible. And in addition to that, my balance was off. I never fell, but I wasn't stable. So we went back to Mayo Clinic and saw Dr. Flanagan again.”
Jim’s relapse was most likely due to his Rituxan treatment being delayed or under-dosed once he was back under care by his local doctors. When he returned to Mayo last March, James again underwent an intravenous steroid (called SOLU-MEDROL) regime for five days, then once a week at home for 12 weeks. After that, the injections were gradually spaced out until he was weaned off them. James also received the Rituxan infusions. Rituxan targets the B cells (and their lineage) in the body, which produce antibodies. The drug is sometimes used to treat leukemia and lymphoma, blood cell cancers that can involve the B cells.
“Rituximab reduces the production of all new antibodies,” says Dr. Flanagan. “But the hope for the patient is that it also reduces those bad antibodies that are making the glycine receptor antibodies.”
The Rituxan, in combination with steroids, worked for James. And that includes his CLL. His bloodwork, checked every six months by his oncologist, has remained stable enough that the CLL hasn’t required additional treatment of any kind.
“THE RITUXAN HELPED WITH ALL OF MY ISSUES,” SAYS JAMES, NOW RETIRED. “AND THE TREATMENT BROUGHT ME IN BALANCE AND REALLY KIND OF CURED EVERYTHING. MY STIFFNESS IMPROVED, I DON’T NEED A WALKER ANYMORE, EVERYTHING IMPROVED. AND IF THINGS GO SOUTH AGAIN, I’LL BE BACK AT MAYO TO SEE DR. FLANAGAN.”
As for James’s treatment and future outlook, Dr. Flanagan is optimistic. “I think we can manage his treatment with the steroids and, mostly, with the rituximab going forward,” he says. “And now that he's on a regular dose of that, he seems to be doing better. So the hope would be to keep him being able to walk and keep him in his best state.”
This article first appeared on the Mayo Clinic Laboratories blog.