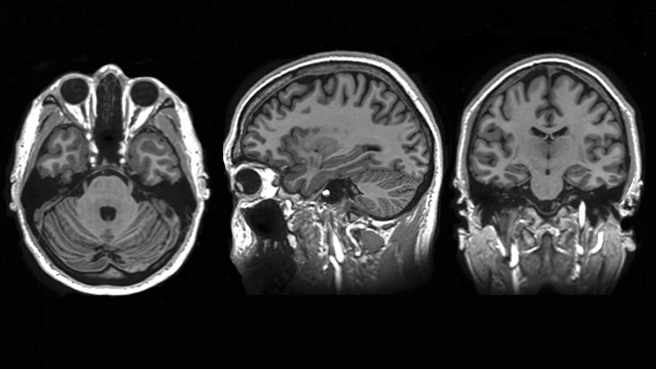
ROCHESTER, Minn. — Patients with three or fewer metastatic brain tumors who received treatment with stereotactic radiosurgery (SRS) had less cognitive deterioration three months after treatment than patients who received SRS combined with whole brain radiation therapy (WBRT). These findings are according to the results of a federally funded, Mayo Clinic-led, multi-institution research study published today in the Journal of the American Medical Association.
“Metastatic brain tumors are unfortunately common in patients with cancer,” says Paul Brown, M.D., a radiation oncologist at Mayo Clinic and the lead author of the study. Dr. Brown says that, while SRS gives physicians the opportunity to treat tumors and spare healthy brain tissue, a combination of SRS plus WBRT has been shown to help control growth of metastatic brain tumors. “The concern is that WBRT also damages cognitive function,” says Dr. Brown. “That is why we have been studying the use of SRS alone.”
Researchers enrolled 213 patients between February 2002 and December 2013, and randomly assigned them to treatment with SRS alone (111) or SRS followed by WBRT (102). Researchers found less cognitive deterioration at three months in patients treated with SRS alone. Quality of life (QOL) was also higher at three months among patients treated with SRS alone. There was no significant difference in functional independence at three months between treatment groups. Median overall survival was 10.4 months for patients treated with SRS alone and 7.4 months for patients treated with SRS and WBRT.
MEDIA CONTACT: Joe Dangor, Mayo Clinic Public Affairs, 507-284 5005, newsbureau@mayo.edu
“This is the first large-scale clinical trial to evaluate this patient population with a comprehensive battery of cognitive and QOL instruments,” Dr. Brown says. “WBRT has often been offered early in the disease course for patients with metastatic brain tumors, but, because of this trial, we know the negative impact of WBRT on both quality of life and cognitive function is significant. With these trial findings, we expect practice will shift, reserving WBRT for patients with more extensive disease in the brain.”
Mayo Clinic co-authors are:
- Kurt Jaeckle, M.D.
- Jane Cerhan, Ph.D.
- Bruce Pollock, M.D.
- Evanthia Galanis, M.D.
- Jan Buckner, M.D.
- Karla Ballman, Ph.D.
Other co-authors are:
- Anthony Asher, M.D., Carolinas Healthcare System
- Elana Farace, Ph.D., Penn State Hershey Medical Center
- Xiomara Carrero, B.S., Alliance Statistics and Data Center
- Keith Anderson, M.S., Alliance Statistics and Data Center
- Fred Barker II, M.D., Massachusetts General Hospital
- Richard Deming, M.D., Mercy Medical Center
- Stuart Burri, M.D., Levine Cancer Institute
- Cynthia Ménard, M.D., Princess Margaret Cancer Center
- Caroline Chung, M.D., Princess Margaret Cancer Center
- Volker Stieber, M.D. Novant Health Forsyth Medical Center
The trial was conducted by the NCCTG (Alliance for Clinical Trials in Oncology) in collaboration with other cooperative groups, including the Radiation Therapy Oncology Group, and was supported by grants U10CA180821, U10CA180882, CA076001, CA025224, RTOG U10CA21661, and NRG U10CA180868 from the National Cancer Institute.
About Mayo Clinic Cancer Center
As a leading institution funded by the National Cancer Institute, the Mayo Clinic Cancer Center conducts basic, clinical and population science research, translating discoveries into improved methods for prevention, diagnosis, prognosis and therapy. For information on cancer clinical trials, call the clinical trial referral office at 1-855-776-0015 (toll-free).
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to clinical practice, education and research, providing expert, whole-person care to everyone who needs healing. For more information, visit http://www.mayoclinic.org/about-mayo-clinic or https://newsnetwork.mayoclinic.org/.







