-
Featured News
Study: Continuous electrical brain stimulation helps patients with epilepsy
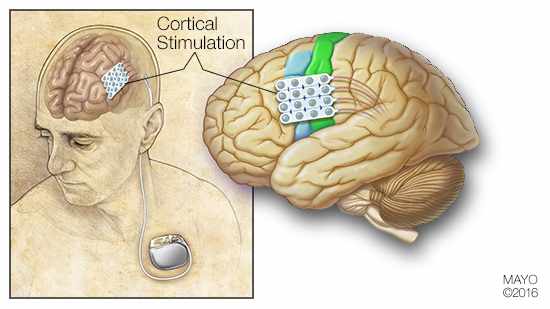 ROCHESTER, Minn. — When surgery and medication don’t help people with epilepsy, electrical stimulation of the brain has been a treatment of last resort. Unfortunately, typical approaches, such as vagal nerve stimulation or responsive nerve stimulation, rarely stop seizures altogether. But a new Mayo Clinic study in JAMA Neurology shows that seizures were suppressed in patients treated with continuous electrical stimulation of the brain's cortex.
ROCHESTER, Minn. — When surgery and medication don’t help people with epilepsy, electrical stimulation of the brain has been a treatment of last resort. Unfortunately, typical approaches, such as vagal nerve stimulation or responsive nerve stimulation, rarely stop seizures altogether. But a new Mayo Clinic study in JAMA Neurology shows that seizures were suppressed in patients treated with continuous electrical stimulation of the brain's cortex.
Epilepsy is a central nervous system disorder in which nerve cell activity in the brain becomes disrupted. In the study, 13 patients with drug-resistant epilepsy were deemed unsuitable for resective surgery, which removes a portion of the brain — usually about the size of a golf ball — that was causing seizures. When patients are evaluated for surgery, a grid of electrical contacts is placed on the brain to record seizures and interictal epileptiform discharges (IEDs). IEDs are electrical discharges that occur intermittently during normal brain function, and have been used as markers to locate portions of brain affected by epilepsy.
In the study, the grid of electrical contacts was used for stimulation at levels the patient would not notice. If the stimulation provided clinical benefit to the patient, this temporary grid was replaced with more permanent contacts that could offer continuous stimulation.
MEDIA CONTACT: Susan Barber Lindquist, Mayo Clinic Public Affairs, 507-284-5005, newsbureau@mayo.edu
Ten of the 13 patients, 77 percent, reported improvement for both epilepsy severity and life satisfaction. The majority of patients experienced more than 50 percent reduction in seizures, and 44 percent were free of disabling seizures. The reduction in IED rate occurred within minutes of initiating stimulation.
“This study suggests that subthreshold cortical stimulation is both effective clinically and reduces interictal epileptiform discharges,” says lead author Brian Lundstrom, M.D., Ph.D., a neurology epilepsy fellow at Mayo Clinic. “We think this approach not only provides an effective treatment for those with focal epilepsy but will allow us to develop ways of assessing seizure likelihood for all epilepsy patients. It would be of enormous clinical benefit if we could personalize treatment regimens for individual patients without waiting for seizures to happen.”
During seizures, abnormal electrical activity in the brain sometimes results in loss of consciousness. For people with epilepsy, seizures severely limit their ability to perform tasks where even a momentary loss of consciousness could prove disastrous — driving a car, swimming or holding an infant, for example. Approximately 50 million people worldwide have epilepsy, according to the World Health Organization.
Seizures sometimes have been compared to electrical storms in the brain. Seizure signs and symptoms may include:
- Temporary confusion
- A staring spell
- Uncontrollable jerking movements of the arms and legs
- Loss of consciousness or awareness
Treatment with medications or surgery can control seizures for about two-thirds of people with epilepsy. However, when drug-resistant focal epilepsy occurs in an area of the brain that controls speech, language, vision, sensation or movement, resective surgery is not an option.
“For people who have epilepsy that can’t be treated with surgery or medication, effective neurostimulation could be a wonderful treatment option,” Dr. Lundstrom says.
The risks of subthreshold cortical stimulation are relatively minimal and include typical infection and bleeding risks as well as the possibility that the stimulation would not be subthreshold and would be noticed by the patient, Dr. Lundstrom says. The authors note that further investigation is needed to quantify treatment effect and examine the effect mechanism. The authors plan to examine the efficacy of this approach in a prospective clinical trial.
This study represents ongoing efforts to restore normal function to epileptic brain tissue by using neurostimulation. Other efforts are aimed at understanding the physiologic changes that chronic stimulation produces in brain tissue.
Study coauthors include Jamie Van Gompel, M.D.; Jeffrey Britton, M.D.; Katherine Nickels, M.D.; Nicholas Wetjen, M.D.; Gregory Worrell, M.D., Ph.D.; and Matt Stead, M.D., Ph.D.
National Institutes of Health grants R01 NS063039 and NIH R01 NS078136 contributed to data collection.
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to clinical practice, education and research, providing expert, whole-person care to everyone who needs healing. For more information, visit http://www.mayoclinic.org/about-mayo-clinic and https://newsnetwork.mayoclinic.org/.







