-
Aging
Taking a Closer Look at Menopausal Hormone Therapy and Cognitive Health
While hormone therapy has been one avenue to address the symptoms associated with menopause, over the years the treatment also has raised a slew of questions.
Back in 2002, the Women's Health Initiative, a massive nationwide study of postmenopausal women, reported that hormone therapy led to an increased risk of breast cancer, stroke, heart attack and dementia. The alarming findings prompted millions of women to avoid hormones, choosing instead to brave the myriad symptoms of menopause, such as hot flashes, sleep problems, mood swings, memory issues, reduced libido and weight gain.
However, since then, several follow-up studies have clarified those initial findings. They even suggest that the benefits of hormone therapy typically outweigh the risks, particularly for younger women who are closer to the menopause transition.
Hormone therapy today is tailored and dosed according to each person's age, stage of menopause and health history, and the treatment is reassessed periodically, says Stephanie Faubion, M.D., the Penny and Bill George Director for the Center for Women's Health. But despite reassuring follow-up findings from the Women’s Health Initiative trials and more recent studies confirming the relative safety of hormone therapy, the media coverage from two decades ago was so disparaging, many women remain afraid to ask for it or to use it. That means many are not getting the help they need.
One key area researchers are investigating is how estrogen therapy affects memory and brain health. Kejal Kantarci, M.D., who’s in the division of neuroradiology and is director of the Women's Health Research Center, became involved in studying the brain effects of hormone therapy more than 15 years ago. The study, known as the Kronos Early Estrogen Prevention Study (KEEPS), found that hormone therapy had no adverse effects on memory and thinking skills.
"There's so much controversy in the field that we had to do this study to shed light into this big question," she says.

Timing Matters for Menopause Studies
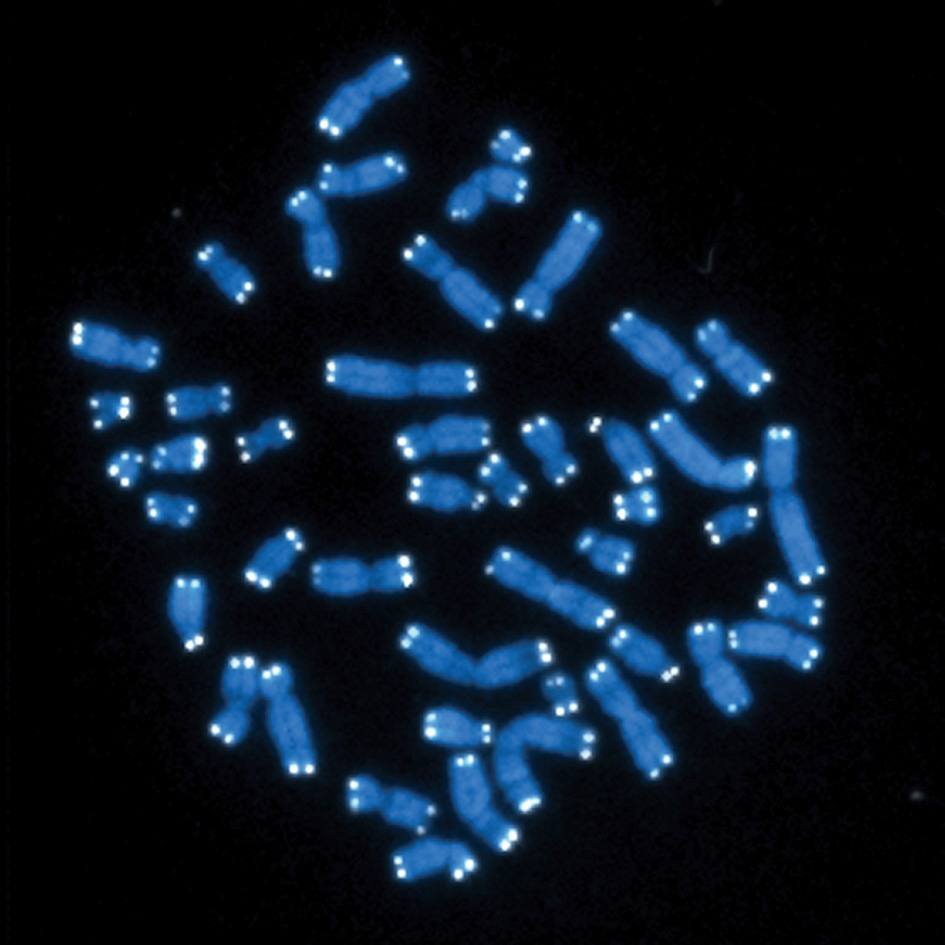
Estrogen is more than just a sex hormone. It plays a vital role in maintaining brain health. The hormone acts directly on brain regions, such as the prefrontal cortex and the hippocampus, that are involved in cognition. In fact, its receptors are scattered throughout the brain, allowing the hormone to exert its effects in countless ways. Dr. Kantarci, whose work is conducted in collaboration with Mayo Clinic's Specialized Center of Research on Sex Differences, has hypothesized that the loss of estrogen during menopause causes the inactivation of those receptors and changes the physiology of the brain.
"That doesn't mean the brain gets worse — it just adapts to the loss of estrogen," says Dr. Kantarci. "And during that adaptation, some individuals get adverse effects, like hot flashes or sleep disturbances that cause them to experience mood changes or cognitive difficulties."
By replenishing the body's stores of estrogen, menopausal hormone therapy can relieve many of menopause's unwanted symptoms.
For decades, women took hormones before the risks and benefits of the therapy were put to the test in the Women's Health Initiative trials. One trial, investigating estrogen plus another hormone, was halted prematurely after results suggested the therapy did more harm than good. A trial of estrogen alone continued. But almost immediately, researchers began poking holes in the study's conclusions. For example, many questioned whether the Women's Health Initiative findings were affected by the fact that most women studied were five or more years beyond menopause.
"I think there is this misinformation or misguidance that came out of the Woman's Health Initiative trials that women who undergo menopause should avoid hormone therapies," says Dr. Kantarci. "While that study demonstrated what happens if you take menopausal hormone therapy at older ages, it did not answer the question of women taking hormone therapies during the menopause transition, which is the time when we really need to address symptoms."
Answer the Question
The KEEPS study was designed to answer that question. In the study, 728 women who were recently postmenopausal were randomly selected to a pill or patch form of estrogen treatment, or matching placebos. Researchers assessed the impact of these treatments on cardiovascular disease, breast cancer, bone health, sexual function and cognition. For her part, Dr. Kantarci used neuroimaging to examine how estrogen affected the brain in the study participants.
Cognitive testing did not show any benefit or risk for hormone therapy on cognitive decline. Interestingly, brain scans found that the rate of aging in the brain's prefrontal cortex actually slowed down in women taking one of the estrogen formulations used in the clinical trial.
To see what cognitive impacts or brain imaging changes might emerge in the research participants later in life, Dr. Kantarci secured funding from the National Institutes of Health and the Alzheimer's Drug Discovery Foundation. She and her colleagues are leading a continuation of KEEPS that will assess the long-term impact of hormones on dementia and Alzheimer's disease in women from the original study.
"We were able to get about a third of the women back for this larger imaging study, even though more than a decade has passed, and this is a more involved study with radioligands, PET (positron emission tomography) scans and MRIs that takes two days to complete all the procedures," says Dr. Kantarci.
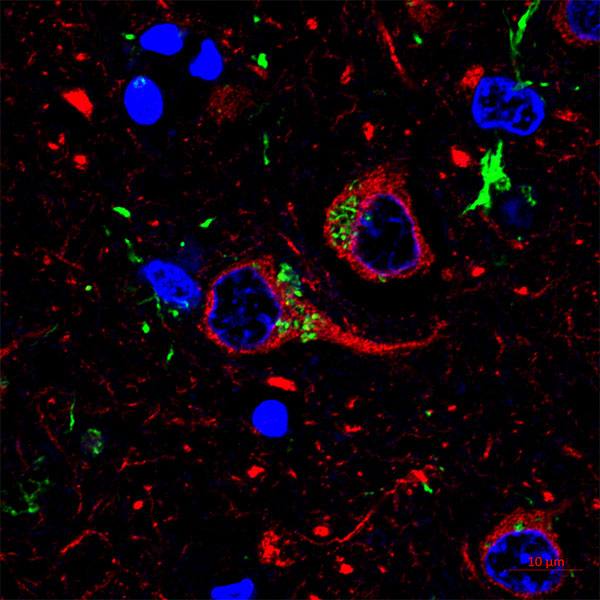
The research team is using radioactively labeled compounds known as radioligands to target and visualize two of the main hallmarks of Alzheimer's disease: amyloid plaques and tau aggregates. These abnormalities accumulate in the brain years before people develop cognitive deficits, enabling researchers to glimpse Alzheimer's and other neurodegenerative diseases at very early stages.
The team expects to have results ready to publish next year. If they detect lower levels of amyloid or tau in women who received hormone therapy, that would suggest the treatment provides some benefit. If they show the opposite, that would be cause for concern. It is also possible that neuroimaging will find no changes, which still would be informative.
"That would mean women could feel safe about using these formulations during the menopausal transition," says Dr. Kantarci. "I think it will be really important, whatever we find, because it will give women information that could help them decide whether or not to use menopausal hormone therapy."
But Dr. Kantarci expects the results to be a bit more complicated than simply all or nothing. "This is complex," she acknowledges. "There's cognition-related changes, brain structure changes, sleep-related changes, Alzheimer's disease changes, white matter changes due to blood vessel disease. Each one of them has a different mechanism in terms of estrogen's effects. So we may see a benefit in one or some, and risk in another."
For women already taking hormone therapy, Dr. Kantarci and Dr. Faubion advise staying the course. Both think the demonstrated benefits outweigh the potential risks and that a generation of menopausal women has missed out on a helpful therapy. Ultimately, Dr. Kantarci hopes the ongoing estrogen research will lead to new hypotheses for preventing any detrimental effects and enhancing the beneficial ones.
"Menopause is not a rare condition," she says. "It's a physiological phenomenon that affects all women, and we need to address it."
—Marla Broadfoot, Ph.D.