-
The BEAUTY of it: award recognizes personalized medicine approach for breast cancer

Back row (from left): Sarah McLaughlin, M.D.; Vera Suman, Ph.D.; Richard Gray, M.D.; Alvaro Moreno-Aspitia, M.D., and Krishna Kalari, Ph.D.
Front row: Liewei Wang, M.D., Ph.D.; Matthew Goetz, M.D.; Judy Boughey, M.D., and Richard Weinshilboum, M.D.
A Mayo Clinic research team supported by the Center for Individualized Medicine is making significant breakthroughs — and gaining recognition for them. The Breast Cancer Genome-Guided Therapy (BEAUTY) project has received the 2019 Mayo Clinic Team Science Award, given for interdisciplinary work that substantially advances Mayo's research. The award cites BEAUTY's discoveries about breast tumor biology and the group's development of lab models, which already are helping to uncover new treatment options for chemotherapy-resistant disease.
Chemotherapy is a standard breast cancer treatment, used for aggressive biology breast cancer to shrink tumors in the breast and lymph nodes before surgery, assess response and destroy any undetected cancer cells elsewhere in the patient. But some breast tumors don't respond well to chemotherapy, putting patients at high risk of recurrence and early death.

New treatments are needed for chemotherapy-resistant breast cancer. But the stunning complexity of breast cancer at the cellular level makes it tough to find alternatives that can target an individual's tumor.
"BEAUTY is a paradigm shift not only in terms of how the trial was designed, but the clinical and research findings that continue to emanate out of the study. We are working to change the standard of care," says Matthew Goetz, M.D., a Mayo medical oncologist who co-leads the project.

The goal is to determine why some patient’s tumors respond to chemotherapy while others don't, and to use that knowledge to develop personalized medicine therapies.
"Breast cancer is not a single disease," says Liewei Wang, M.D., Ph.D., PI of Mayo's Pharmacogenomics and Drug Targets Laboratory and a member of BEAUTY's executive team. "Breast tumors are highly heterogeneous. Every patient experiences a different disease process, so naturally we shouldn't treat every patient the same."
Launched in 2011, BEAUTY has impact beyond Mayo Clinic. The wealth of clinical, genomic and imaging data gathered by the project is being used in multiple collaborations across the nation to guide cancer research. BEAUTY has generated four clinical trials, two patents, multiple NCI and DOD grants, as well as a methodology for incorporating molecular sequencing data into clinical trial results.
"BEAUTY works predominantly to further treatments for breast cancer, however there have also been advantages for some of the individuals enrolled in the study," says Judy Boughey, M.D., a Mayo breast surgeon who co-leads BEAUTY. "We've been able to achieve that because we have a huge multidisciplinary team of clinicians and basic scientists with everyone working together for the greater good."

Germline screening for genetic mutations was performed on blood samples from study participants in BEAUTY.
"In the 124 women, we identified 28 deleterious mutations across 26 patients. That was a lot higher than we expected because this wasn't a group of women with a strong family history of breast cancer," Dr. Boughey says. "In addition to BRCA1 and BRCA2, we found some lesser- known mutations, some of which weren't specific to breast cancer."
Participants with clinically actionable mutations were referred to genetic counselors. "Some of these patients have gone on to get screening for other malignancies that they are at elevated risk of developing in the future," Dr. Boughey says. "That's been an unanticipated benefit of patients' participation in the study."
A chemotherapy-resistant model of success
BEAUTY has resulted in a series of further laboratory and clinical studies of women with invasive breast cancer who qualify for chemotherapy before surgery.
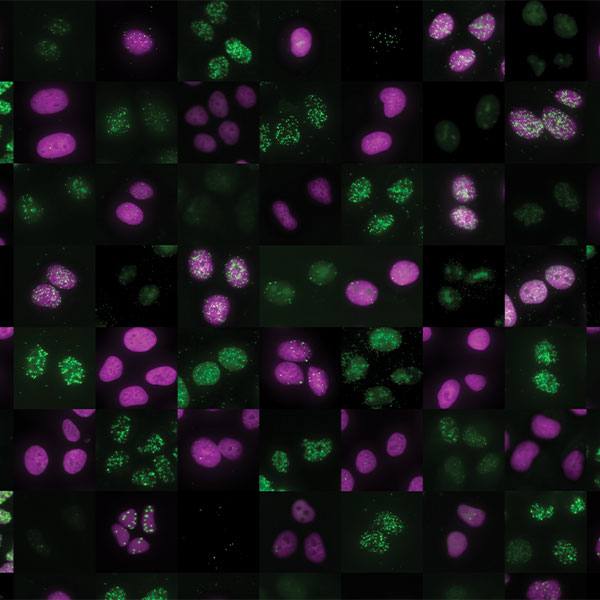
Tissue samples were obtained from BEAUTY participants through minimally invasive needle biopsy. In addition to performing exome and RNA sequencing of the tumors, the researchers achieved a milestone: the successful implantation of patient tumor tissue in laboratory mice to create a living model of an individual's disease, known as a patient-derived xenograft (PDX).
PDXs provide opportunity to further interrogate the tumors, studying the impact of new drugs and drug combinations, and facilitate preclinical studies of new therapies. The BEAUTY team created PDXs from tumor tissue biopsies taken throughout the breast cancer treatment process. That allows the researchers to study the molecular evolution of cancer over the course of treatment and to identify mechanisms of resistance to chemotherapy.
"It's really fortuitous to have PDXs from not only the tumor that's never been exposed to chemotherapy, but also the tumor collected at surgery that continued to remain viable despite being exposed to 20 weeks of chemotherapy. That's truly a chemotherapy-resistant model" Dr. Goetz says. "These are the models that will provide some of the most useful information when it comes to prioritizing new drugs”
BEAUTY's comprehensive genomic and PDX data has led to several discoveries — including a potential treatment for triple negative breast cancer, one of the most aggressive and lethal forms of the disease. "Triple negative" means the tumor lacks the three most common proteins known to respond to existing therapies.
The BEAUTY team found that a drug already approved for treating certain blood cancers can significantly inhibit the growth of some chemotherapy-resistant triple negative breast tumors. The Mayo researchers are now collaborating with the National Cancer Institute to refine the existing drug and plan to launch a clinical trial in women with triple negative breast cancer.
"These new discoveries can lead to more clinical trials that will provide additional choices for personalized care," says Dr. Wang.
Stay informed
Want to read more stories like this one?
Register to get weekly updates about new stories on Mayo Clinic Center for Individualized Medicine blog.
Join the conversation
For more information on the Mayo Clinic Center for Individualized Medicine, visit our blog, Facebook, LinkedIn or Twitter at @MayoClinicCIM