-
 Cancer
CancerTissue Testing During Breast Cancer Lumpectomies Prevents Need for Reoperation 96 Percent of Time
Real-time tissue analysis gives Mayo Clinic much lower reoperation numbers than national rate
 ROCHESTER, Minn. — Unique laboratory testing during breast cancer lumpectomies to make sure surgeons remove all cancerous tissue spares patients the need for a repeat lumpectomy in roughly 96 percent of cases at Mayo Clinic in Rochester, a success rate much higher than the rate nationally, a Mayo study shows. During the years reviewed, 13.2 percent of breast cancer lumpectomy patients nationally had to return to the operating room within a month of their initial surgery, compared to 3.6 percent at Mayo in Rochester, which uses a technique called frozen section analysis to test excised tissue for cancer while patient are still on the operating table. The findings are published in the journal Surgery.
ROCHESTER, Minn. — Unique laboratory testing during breast cancer lumpectomies to make sure surgeons remove all cancerous tissue spares patients the need for a repeat lumpectomy in roughly 96 percent of cases at Mayo Clinic in Rochester, a success rate much higher than the rate nationally, a Mayo study shows. During the years reviewed, 13.2 percent of breast cancer lumpectomy patients nationally had to return to the operating room within a month of their initial surgery, compared to 3.6 percent at Mayo in Rochester, which uses a technique called frozen section analysis to test excised tissue for cancer while patient are still on the operating table. The findings are published in the journal Surgery.
Frozen section analysis was pioneered at Mayo Clinic more than 100 years ago and is used in a variety of Mayo surgeries.
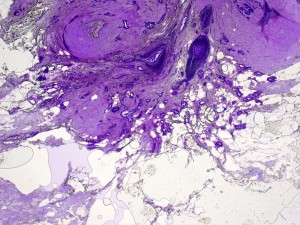
In breast cancer lumpectomies, surgeons remove tumors with a small amount of normal tissue around them to help ensure they excised all of the cancer. This is known as obtaining “clean” or “negative” margins. During surgery at Mayo in Rochester, that tissue is transferred from the operating room to a nearby pathology lab, where the edges around the lumpectomy are shaved and each sample is frozen and reviewed under a microscope by a pathologist, all within minutes, while the patient is still anesthetized. The pathologist immediately gives the surgeon the results, so the surgeon knows whether the lumpectomy is complete or there is still cancerous tissue to remove, and at which margin, before the operation concludes.
Mayo Clinic remains one of the only U.S. medical centers to perform frozen section analysis, and its process is unique, including use of a Mayo-modified microtome to freeze tissue so the pathologist can get a 360-degree view around the lumpectomy cavity.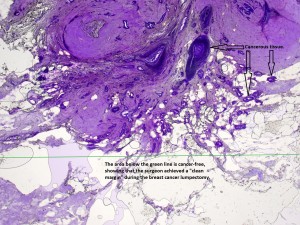
“This intense pathological evaluation with the use of frozen section of the margins while the patient is asleep really drops down the re-excision rate,” says first author Judy Boughey, M.D., a breast surgeon in the Mayo Clinic Cancer Center. “Achieving negative margins in one operation has a huge impact on the patient’s satisfaction, decreases time away from work, time traveling back and forth to hospital appointments, and the financial cost to the patient, the insurance company and the hospital for a second operation.”
Mayo researchers compared 30-day reoperation rates for breast cancer lumpectomy patients at Mayo Clinic in Rochester with the reoperation rates for such patients at hospitals nationally as reported in American College of Surgeons National Surgical Quality Improvement Program data from 2006-10.
Patients in the national data were roughly four times likelier to undergo reoperation as those at Mayo in Rochester. The 30-day reoperation rate after lumpectomy for cancer was 13.2 percent nationally and 3.6 percent at Mayo in Rochester, the analysis found.
Unlike mastectomy — breast removal — a breast cancer lumpectomy typically preserves enough breast tissue to achieve an acceptable cosmetic result. Most women diagnosed with breast cancer have a choice between a lumpectomy and a mastectomy. However, women who have a lumpectomy and later learn another operation is needed to obtain negative margins may decide to get a mastectomy at that point, Dr. Boughey says.
The study’s senior author is Elizabeth Habermann, Ph.D., associate scientific director of the Surgical Outcomes Program in the Mayo Clinic Kern Center for the Science of Health Care Delivery. Mayo Clinic funded the research.
Journalists: Sound bites from Dr. Boughey are available in the downloads below. Click here to download the frozen section margin analysis image with text. Click here to download the frozen section margin analysis image without text.
###
About Mayo Clinic
Recognizing 150 years of serving humanity in 2014, Mayo Clinic is a nonprofit worldwide leader in medical care, research and education for people from all walks of life. For more information, visit 150years.mayoclinic.org, MayoClinic.org or https://newsnetwork.mayoclinic.org/.
MEDIA CONTACT: Sharon Theimer, Mayo Clinic Public Affairs, 507-284-5005, Email: newsbureau@mayo.edu







