-
Tracking Melanoma to Discover New Hope for Patients
This story starts with melanoma. The name of this cancer tells us it grows from skin cells called melanocytes. When these cells break, normal controls fail. The melanocytes divide and grow uncontrollably, burrowing through the layers of skin in a quest to spread. Melanoma of the skin is common, even among people who are in their 40s and therefore less likely to get this or any other cancer before 60. But melanocytes are not confined to our skin. These cells also exist in our mucous membranes, ears, eyes and brain. Melanoma in these cells sometimes is called "hidden melanoma."
A pretty dirty trick, right? The other dirty trick melanoma plays: Sometimes even those given a clean bill of health find that their cancer returns ─ even years later. Patients and families wonder, how could this happen? That is the question researchers and physicians ask, as well: How does this happen?
And how can we stop it?

Stealth and Subterfuge
Svetomir Markovic, M.D., Ph.D., a Mayo Clinic melanoma specialist and researcher, spends his days toggling between seeing patients and researching their disease. He says the easiest way for cancer to spread is through the same channels the immune system uses. What he's referring to is the lymph system, a network of tissues and vessels that collect, drain and clean lymph fluid. Seeping in from tissues and the space between cells, the lymph fluid contains cells, proteins and antibodies among other things. The lymph fluid flows through a network of microscopic tubes, eventually collecting in large chambers called lymph nodes. In these chambers, white blood cells prepare to devour invaders of all sorts, as well as internal threats like cancer.
"The immune system's job is to destroy cancer," Dr. Markovic explains.
But strangely the first place a tumor usually spreads to is the nearest lymph node. For certain stages of melanoma, part of standard medical care is to take a biopsy of that lymph node, called the "sentinel node," to check for cancer cells.
"That lymph node should be the headquarters of the immune response," says Dr. Markovic, but it's not. With melanoma, his lab was surprised to find that the sentinel lymph node and the tissue around it have lower immune cell activity than expected. It is immune suppressed.
In 2012, when Ph.D.-candidate Rachel Maus arrived in the Markovic lab, that intrigued her, as well. With funding from various sources, including Mayo Clinic's Center for Biomedical Discovery, she started investigating.
"This suppressed immune profile was present even in lymph nodes with no melanoma cells present, so there needed to be something coming prior to the cancer cell setting the stage, and that's when our interest turned to extracellular vesicles," says Dr. Maus, who graduated with her doctorate degree from the Mayo Clinic Graduate School of Biomedical Sciences in 2017.
Identifying the Mole
Vesicles are not a new thing. They are membrane-bound sacs that travel among cells. First discovered in 1967, vesicles have been frequently mischaracterized as dust and junk until someone (three someones actually) won a Nobel Prize for figuring out what they do. Dr. Markovic explained it very simply: Just as a box protects its cargo, an extracellular vesicle provides protection for information traveling to and from cells.
"Cells within an organ must communicate beyond their immediate locations," he says. "A lot of the environment around the cells [extracellular] is unfriendly to cell signaling to cut down on noise. Otherwise, nothing would function. Extracellular vesicles allow for needed communication at a distance."
Could vesicles act as moles or spies, affecting the immune response by tricking the immune system, the team wondered?
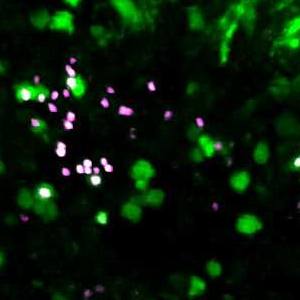
To find out, Dr. Maus grew three melanoma cell lines. The team collected the vesicles from the tumors and looked at both the cargo and how the vesicles affected the immune first responders called dendritic cells.
"I found that the vesicles from the melanoma tumors were shutting down development of the dendritic cells," she says, but they didn't know exactly how. To figure that out, Dr. Maus broke open the vesicles from the tumors. She identified 21 proteins that were shared among all three tumor lines. But when she looked to see if the proteins had known effects on dendritic cells, the results were mixed. You can read the full results in Frontiers in Immunology.
The cargo did not seem to have a clear, singular purpose. It may be, Dr. Maus explains, that just one of the tools (proteins) or instructions (DNA/RNA) sent might drown out the changes in activity from the other items. But the researchers still don't know for sure.
Melanoma signaling may be even sneakier than that.
Peak Sneakiness
When it comes to communication, cancer cells may not be using a cloaking device, but instead may be deep cover agents, hiding among normal cells and recruiting others to send soothing signals to the immune system.
"The melanoma cells at the site of the primary tumor are interacting with all sorts of other cells at that site," explains Dr. Maus. "So it might not be that the melanoma cell is secreting the factor that's going to the lymph node, but instead the melanoma cells might be talking to their neighbors that are still normal cells and causing them to secrete a factor that changes the microenvironment."
That level of complexity might be what keeps the immune system in the dark about the tumor, says Dr. Maus.
"If the melanoma cell sent a signal to the lymph nodes, and it shouted that it was a tumor, the immune cells would kill it," she says. "So the tumor has to be more discreet. It has to slowly shut down the lymph node to where it can no longer react. And that's when the tumor cell can come in and set up camp."
And that, Dr. Maus explains, is what they are trying to find for patients: a biological signature in the lymph node that pathologists can screen for at the time of biopsy.
Your Mission Should you Choose to Accept it
"Right now, the biopsy is relatively simplistic: Is there a tumor cell in the lymph node or not," she explains. But cancer isn't that binary. People whose biopsy comes back positive for a cancer cell in the lymph node may go on to be cancer-free forever, while someone else with a negative biopsy can develop metastatic disease two years later.
"So our next step was to try and clarify that transition, and find more clues about what's happening in the lymph nodes," says Dr. Maus.
To do that, the team needed to collect not just the lymph node, but also the lymph channel and, by extension, the fluid within it that drains into that node. It's no small feat. Lymph channels are, by definition, leaky ─ not to mention microscopic. But to be a melanoma researcher is to be hopeful for the future, and the team was undeterred.
"We were fortunate to find something that we did not expect, fortunate to have a young scientist who came up with a brilliant concept and fortunate to have the tools to test this. And we said, you know, we are in a unique position to address a very critical problem," says Dr. Markovic.
So they did what many researchers at Mayo do: reach out for help.
"Some people here say the most useful part of Mayo is the phone," quips Dr. Markovic. "We had a colleague that we saw every day, and I kind of cornered him at one point and asked him, 'What you think about this idea?'"
That colleague was James Jakub, M.D., a Mayo Clinic surgeon.

Setting up the Sting
Like Dr. Markovic, Dr. Jakub is a physician-researcher interested in expanding knowledge of lymph node biology and how disease gets a foothold in the node.
"We talk across the practice and research aisle every day about patients; formally, informally curbside, in emails," says Dr. Jakub. "The clinical work and the research work overlap on a number of projects that have to do with lymph node biology and cancer."
So when approached by Dr. Markovic, Dr. Jakub was open to collaboration. The first step though, says Dr. Jakub, was scaling the "tremendous logistical mountain" to obtain tissue for analysis. And he says it hinged on their unique collaboration with the pathology team.
"Most places would not be able to make this work and keep the patient safe," says Dr. Jakub. "We can do it because our pathology team is so good that this process does not compromise routine patient staging and pathologic evaluation."
So with the logistical mountain scaled, all Dr. Jakub had to do was figure out how to harvest a microscopic vessel along with the fluid that typically leaks out of it from the part of the system that drains into the node and not out of it.
Tracking the Mark
Drainage from cells isn't random, says Dr. Jakub.
"It's like train tracks, so it's going into the same station every time, and it's predictable," he explains. "That has been described since the 1990s." To identify where the tumor drains, the nuclear medicine team inject a radioactive tracer into the area around the tumor. They watch it drain and take an X-ray to show the pathway.
In surgery, Dr. Jakub says, they have two ways to see that spot.
"One is audible using a probe that counts radiation and beep-beep-beeps, kind of like 'Star Trek,'" he says. "The other is visual, where blue dye shows the channel that's draining into the lymph node because, with just the sound, you wouldn't know which channel was coming into it and which is going out."
"We have magnifying loupes and small dissectors and clips. We clip each side of the lymphatic channel and seal in the fluid, cut that little channel out, and that's what goes to the research lab."
Dr. Maus and team then take that fluid, along with fresh lymph node tissue and blood drawn from the same patient, and look to see if immune suppression is occurring.
"All these ideas that we've had and validated in previous studies, we can continue with and now that we have the lymphatic channel coming from the same patient from which we also get a preop blood draw, we have all of the pieces," says Dr. Maus, " which gives us a great model and a great system to work in to test new hypotheses that we're generating."
And that, says Dr. Jakub, brings up an important point.
"None of this would be possible without the patients," he says. "I just saw a patient today, and her exact words were, 'I know this is not going to help me, but I want it to help my grandchildren.' Agreeing to be in the study adds no value to the patient's care as an individual, but they are altruistic, and they want to advance the treatment of cancer. And without them, none of this would be possible."
This story is undoubtedly about melanoma ─ one of the trickiest, sneakiest cancers we face. But it's also about the how the mystery of melanoma is being solved with the help of research students, scientists, physicians and patients together. So, really, it's about the end of melanoma.
Wouldn't we all like to see that?
─ Sara Tiner