DEAR MAYO CLINIC: I am 52 and have been diagnosed with dry macular degeneration. What could cause this in a person my age?
 ANSWER: No one knows exactly what causes macular degeneration, an eye disease that can lead to loss of sight in the center of your field of vision. But the risk for macular degeneration goes up as you get older. Other factors play a role, too. A family history of the disease, race, lifestyle choices such as smoking and diet, and underlying medical conditions can all increase the likelihood of developing macular degeneration.
ANSWER: No one knows exactly what causes macular degeneration, an eye disease that can lead to loss of sight in the center of your field of vision. But the risk for macular degeneration goes up as you get older. Other factors play a role, too. A family history of the disease, race, lifestyle choices such as smoking and diet, and underlying medical conditions can all increase the likelihood of developing macular degeneration.
The macula is the part of your eye that allows you to see fine details in your vision. You need it for tasks such as driving, reading and recognizing faces. The macula is located in the center of your retina — the layer of tissue on the inside back wall of your eyeball.
There are two kinds of macular degeneration. The kind you have, dry macular degeneration, is more common. It happens when retinal cells in the macula die, causing the macula to break down. The other form of this disease is called wet macular degeneration. That happens when blood vessels under the retina leak blood and fluid into the macula.
Some of the risk factors for macular degeneration are beyond your control. For example, the older you are, the more likely you are to develop macular degeneration. The disease is most common in people older than 65, but the risk begins to go up significantly beginning around age 50.
Genetics appear to have an effect, too. If someone in your family had macular degeneration, then you are more likely to develop it. Race also makes a difference. Macular degeneration is more common in Caucasians than it is in other races.
There are other risk factors, however, that you can control. People who don’t smoke are less likely to develop macular degeneration than people who do. Maintaining a healthy weight and eating a healthy diet lower the risk, too. Effectively managing other chronic health problems, such as high blood pressure, heart disease and high cholesterol, also can make macular degeneration less likely.
Even after the diagnosis of macular degeneration, there are still steps you can take that may help slow vision loss, including a range of healthy diet choices. Research has shown that vitamins A, C and E, along with zinc and copper, are particularly beneficial for people who have macular degeneration. With that in mind, eat lots of fruits and vegetables every day. The wider the range of the fruits and vegetables, the more variety of vitamins you will have in your diet.
Omega-3 fatty acids also may help reduce the risk of vision loss related to macular degeneration. Omega-3 fatty acids are best consumed from nutritional sources rather than supplements. They can be found in fish, such as salmon, sardines and tuna, and nuts such as walnuts.
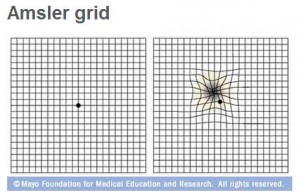
It is important that you look for changes in your vision using an Amsler grid. The grid is much like a crossword puzzle grid. You should check each eye separately by covering up the other eye. If the lines appear wavy or are missing, it could mean that either the dry macular degeneration has progressed, or that the dry has converted to the wet form. The wet form means there is a blood vessel growing under the macula. This needs prompt treatment, most commonly with medications injected into the eye, starting on a monthly basis. Prompt intervention can treat this unwanted blood vessel and slow down or even improve your vision.
Talk to your doctor about diet choices that may be appropriate for you, as well as other treatment options for macular degeneration. Increasing your vitamin intake through supplements could be useful in slowing vision loss. Although treatment cannot reverse the effects of dry macular degeneration, that does not mean you will lose all of your vision. In many cases, the disease progresses slowly, and people are often able to perform many of their day-to-day activities even though they have macular degeneration. — Sophie J. Bakri, M.D., Ophthalmology, Mayo Clinic, Rochester, Minn.
Related Articles







