-
Transplant
(VIDEO) When to consider a lung transplant: A Mayo Clinic expert explains
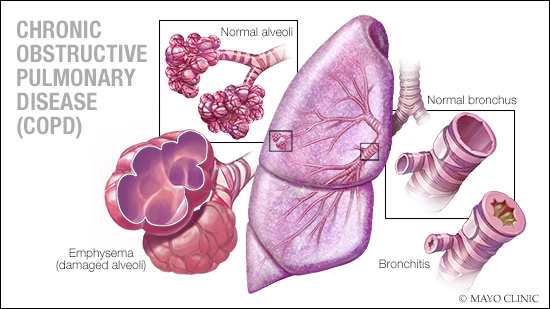
Chronic obstructive pulmonary disease (COPD), emphysema and pulmonary fibrosis are serious respiratory conditions that, when they progress to advanced stages, can significantly impair lung function and overall health. A lung transplant may be considered to prolong life and improve quality of life when standard treatments are no longer effective.
Dr. Maher Baz, a Mayo Clinic transplant pulmonologist, says a lung transplant is a complex and major surgery that can significantly improve a patient's survival and quality of life.
Watch: Dr. Maher Baz discusses lung transplantation
Journalists: Broadcast-quality sound bites with Dr. Baz are available in the downloads at the end of the post. Please courtesy: "Mayo Clinic News Network." Name super/CG: Maher Baz, M.D./Transplantation Medicine/Mayo Clinic.
When it's time for a lung transplant
A lung transplant is typically considered when a patient's disease severely impacts day-to-day functioning and/or threatens survival.
“About 30% to 40% of those who need a lung transplant have late-stage chronic obstructive pulmonary disease and need quality-of-life care,” Dr. Baz says.
Lung transplantation for patients with pulmonary fibrosis, emphysema or COPD can greatly improve overall health. For many, a transplant reduces dependence on oxygen, helping them live more active and independent lives.
"We feel that their quality of life will improve significantly after the transplant. Because they're no longer on oxygen, they can be out and about, walk farther, go on vacations and improve their survival," says Dr. Baz. "There's a subpopulation, especially for fibrosis; we think we can add several years to their survival.”
Advancements in lung transplantation
Medical innovation has dramatically evolved the lung transplant process, making transplants safer and more effective for patients. One of the most significant advances is a system that tests and preserves donated lungs.
"We have something called ex vivo lung perfusion, or EVLP. It's where we put the donated lungs on a breathing machine, circulate fluid in them, test them for about three to four hours and ensure they are good lungs," Dr. Baz explains.
This method ensures donated lungs are viable for transplantation, significantly boosting the availability of usable organs. It means shorter wait times and more opportunities to find suitable donors.
Improved care
Thanks to improved personalized patient care, rehabilitation, infection management and rejection treatment advancements, both short-term and long-term survival rates for lung transplants have improved significantly.
Transplant, says Dr. Baz, can be life-transforming. "It will take patients from being dependent on oxygen, dependent physically, to independent of oxygen and an independent lifestyle. And it can do that often within a few weeks after transplant surgery."
It's important to note that a lung transplant isn't right for everyone. Many factors determine eligibility, so working closely with your care team to evaluate the best treatment option is important.
Related posts:
- A journey of resilience and hope
- Mayo Clinic’s transplant center in Florida reaches 800th lung transplant milestone, on track for record-setting year







