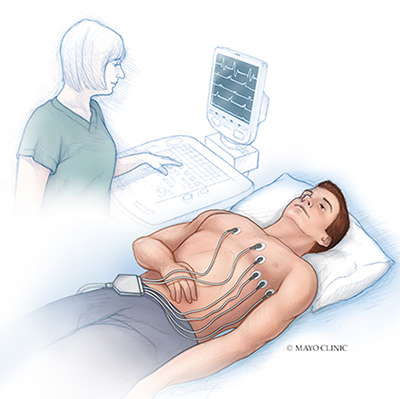
Diagnosing for sick sinus syndrome might include:
- Electrocardiogram (ECG). During this test, sensors (electrodes) are attached to your chest and limbs to create a record of the electrical signals traveling through your heart. The test might show patterns that indicate sick sinus syndrome, including fast heart rate, slow heart rate or a long pause in the heartbeat (asystole) after a fast heart rate.
- Holter monitor. This portable device is carried in your pocket or in a pouch on a belt or shoulder strap. It automatically records your heart's activity for 24 to 72 hours, which provides your health care provider with an extended look at your heart rhythms.

- Event recorder. This portable electrocardiogram device can also be carried in your pocket or worn on a belt or shoulder strap for home monitoring of your heart's activity. You might be asked to use this device to use for up to a month.When you feel symptoms, you push a button, and a brief ECG recording is saved. This allows your health care provider to see your heart rhythm at the time of your symptoms, which can help pinpoint sick sinus syndrome.
- Implantable loop recorder. This small device is implanted just under the skin of your chest and is used for continuous, long-term monitoring of your heart's electrical activity. An implantable loop recorder may be worn from months to years.This device is automatically triggered by an irregular heart rhythm (arrhythmia) or you can trigger it when you feel symptoms.
Treatment
Treatment for sick sinus syndrome focuses on eliminating or reducing unpleasant symptoms. If you aren't bothered by symptoms, you may only need regular checkups to monitor your condition. For people who are bothered by symptoms, the treatment of choice is usually an implanted electronic pacemaker.
Medication changes
Your health care provider will likely check your current medications to see if any could be interfering with the function of your sinus node. Medications used to treat high blood pressure or heart disease — such as beta blockers or calcium channel blockers — can worsen abnormal heart rhythms. In some cases, adjusting these medications can relieve symptoms.
Pacing the heart
Most people with sick sinus syndrome eventually need a permanent artificial pacemaker to maintain a regular heartbeat. This small, battery-powered electronic device is implanted under the skin near your collarbone during a minor surgical procedure. The pacemaker is programmed to stimulate or "pace" your heart as needed to keep it beating normally.
The type of pacemaker you need depends on the type of irregular heart rhythm you have. Some rhythms can be treated with a single chamber pacemaker, which uses only one wire (lead) to pace one chamber of the heart — in this case, the atrium. However, most people with sick sinus syndrome benefit from dual chamber pacemakers, in which one lead paces the atrium and one lead paces the ventricle.
You'll be able to resume normal or near-normal activities after you recover from pacemaker implantation surgery. The risk of complications, such as swelling or infection in the area where the pacemaker was implanted, is small.
Additional treatments for fast heart rate
If you have a rapid heart rate as part of your sick sinus syndrome, you may need additional treatments to control these rhythms:
- Medications.
If you have a pacemaker and your heart rate is still too fast, your doctor may prescribe anti-arrhythmia medications to prevent fast rhythms. If you have atrial fibrillation or other abnormal heart rhythms that increase your risk of stroke, you may need a blood-thinning medicine, such as warfarin (Coumadin, Jantoven) or dabigatran (Pradaxa).
- AV node ablation.
This procedure can also control fast heart rhythms in people with pacemakers. It involves applying radiofrequency energy through a long, thin tube (catheter) to destroy (ablate) the tissue around the atrioventricular (AV) node between the atria and the ventricles. This stops fast heart rhythms from reaching the ventricles and causing problems.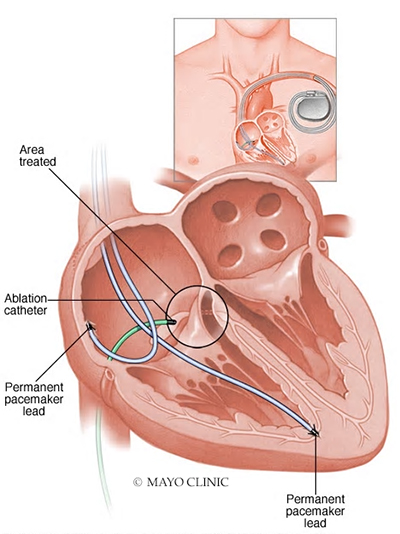
- Radiofrequency ablation of atrial fibrillation.
This procedure is similar to AV node ablation. However, in this case, ablation targets the tissue that triggers atrial fibrillation. This actually eliminates atrial fibrillation itself, rather than just preventing it from reaching the ventricles.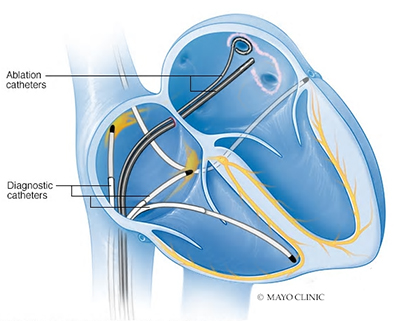
This article is written by Mayo Clinic staff. Find more health and medical information on mayoclinic.org.