The delta variant is now believed to be responsible for more than 80% of the new COVID-19 infections diagnosed in the U.S. But to be diagnosed with COVID-19, you must first be tested.
Watch: Dr. Bobbi Pritt discusses COVID-19 tests
Journalists: Broadcast-quality sound bites are in the downloads at the bottom of the page. Please courtesy: "Bobbi Pritt, M.D./Microbiology/Mayo Clinic."
The Mayo Clinic New Network team sat down with Dr. Bobbi Pritt, chair of Mayo Clinic's Division of Clinical Microbiology. In this Q&A, Dr. Pritt explains the various COVID-19 tests, what they do and what these tests detect:
What types of COVID-19 tests are used?
Two main types of tests are used. We have tests that are good at detecting active infection when someone may have symptoms or was recently exposed to someone who was infected. Those tests are the polymerase chain reaction and antigen tests. Then we have the other type of test, which is very good at detecting evidence of past infection. We call these tests serology tests, and they detect antibodies.
The polymerase chain reaction and antigen tests are both done on a nasal swab specimen. The polymerase chain reaction test detects the virus' genetic code ― its molecular material ― which in the case of this virus is RNA. It's detecting the virus' genetic code that it uses to replicate itself and make more virus. The antigen test detects proteins from the virus rather than molecular information. It's looking at the proteins that make up the virus.
The other type of tests ― the serology test or antibody test that use a blood draw ― you get a blood specimen, and that specimen is tested for evidence of past inspect infection. The antibody test detects your own hosts' immune response, your own body's response to fighting off the virus by detecting something called antibodies. That's the part of your immune response that helps attack foreign invaders like viruses.
What does it mean if someone has a high viral load when tested?
The viral load refers to the amount of virus that we have in our bodies. But when people say high viral load, it typically refers to the amount of virus that's detected in that nasal swab through testing, usually by polymerase chain reaction. Now polymerase chain reaction can give us a general indication for how much virus is present in that sample. Although usually it doesn't measure the specific amount, we can get a general idea if the patient has a high viral load, or a low or moderate viral load. Now why is this important? If someone has a high viral load, they are potentially shedding that virus into the environment. And they could be infectious to others. They could transmit that virus to other people around them.
Can a polymerase chain reaction test mistake the influenza virus for COVID-19?
The COVID-19 tests on the market that have been reviewed by the Food and Drug Administration are very specific for COVID-19. They don't give you a false positive if you had influenza, for example. They're specific only for SARS-CoV-2, which is the virus that causes COVID-19.
Does COVID-19 testing determine whether your infection is caused by the delta variant, and does infection by the delta variant affect treatment?
The test that most people receive will not tell them what variant they have. It will just be a yes or no answer. They either have the virus or they don't in the specimen that was tested. There's another test that we can perform to see what variant people have. But it's not usually performed for patient care, meaning that it's not usually important for how the patient's going to do clinically. It's something more that our public health officials want to know so that they can monitor the spread of the virus and the different variants throughout our community.
When should a person be tested for COVID-19?
If someone has symptoms that are consistent with COVID-19, they should be tested. If they've also been exposed to someone who has proven COVID-19, the recommendation is now for them also to be tested, even if they've been vaccinated.
How effective are COVID-19 vaccines against the delta variant?
Speaking just about the vaccines we have in the U.S., studies have thankfully shown that they are still very good at protecting us against the delta variant. It looks like it is greater than 85% effective in protecting us against symptomatic infection. Even with the delta variant, the efficacy is a little less to become infected without symptoms, but the chance of you getting ill is low. And the risk of needing hospital care is even lower of you getting a very serious infection where you have to go to the hospital. The bottom line is still this: Vaccination is very effective against the delta variant.
____________________________________
For the safety of its patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was either recorded prior to COVID-19 or recorded in a nonpatient care area where social distancing and other safety protocols were followed.
Information in this post was accurate at the time of its posting. Due to the fluid nature of the COVID-19 pandemic, scientific understanding, along with guidelines and recommendations, may have changed since the original publication date.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org.
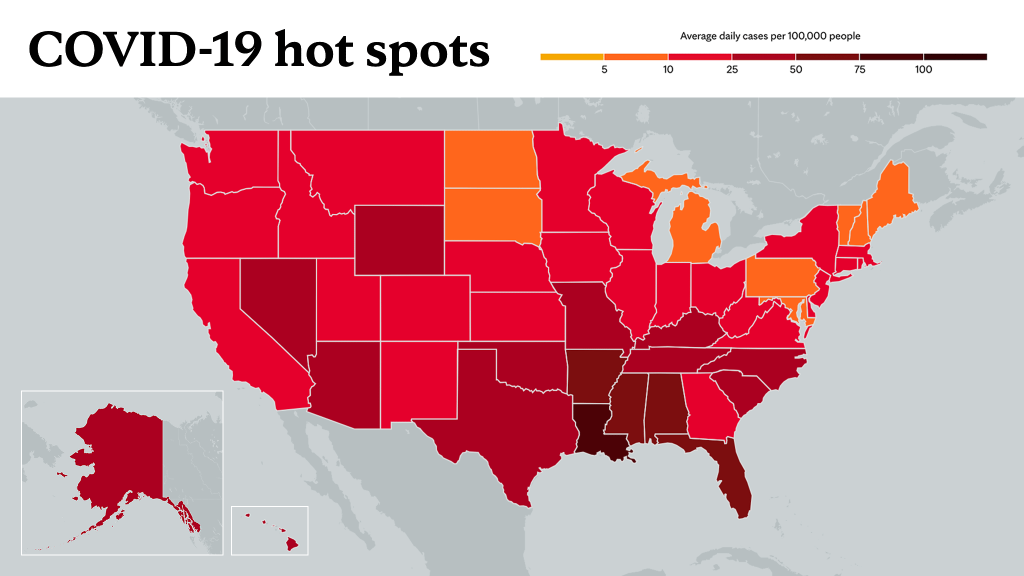
Learn more about tracking COVID-19 and COVID-19 trends.