 DEAR MAYO CLINIC: After a recent mammogram, my doctor suggested an additional test. She recommended molecular breast imaging, but, when I got to the appointment, I was scheduled for 3-D imaging. What is the difference between the two? Is one more accurate than the other at detecting breast cancer?
DEAR MAYO CLINIC: After a recent mammogram, my doctor suggested an additional test. She recommended molecular breast imaging, but, when I got to the appointment, I was scheduled for 3-D imaging. What is the difference between the two? Is one more accurate than the other at detecting breast cancer?
ANSWER: Both molecular breast imaging and a 3-D mammogram, also called tomosynthesis, can help doctors see inside the breast more clearly than they can with standard mammography. But the two tests are different in the way they image the breasts.
Tomosynthesis is an anatomic test. That means cancer is seen based on changes in how the breast anatomy looks. Getting a tomosynthesis feels the same as getting a standard mammogram. Your breast is compressed, and X-rays pass through the breast to make pictures of your breast tissue.
However, rather than an image that is formed from pictures taken from top to bottom and side to side, like a conventional, two-dimensional mammogram, a 3-D mammogram takes multiple thin pictures of the breast. With the 3-D approach, the breast tissue can be analyzed layer by layer. This reduces overlapping tissue, which is a common reason women are brought back for extra pictures after a standard screening mammogram.
Research shows tomosynthesis can detect more breast cancers than standard mammography. It’s useful for women with dense breast tissue, because the thin pictures can make a cancer easier to see through the dense breast tissue.
Molecular breast imaging also has been shown to be valuable for women with dense breast tissue. Molecular breast imaging, when combined with a standard mammogram, detects more breast cancers in women with dense breast tissue than a mammogram alone.
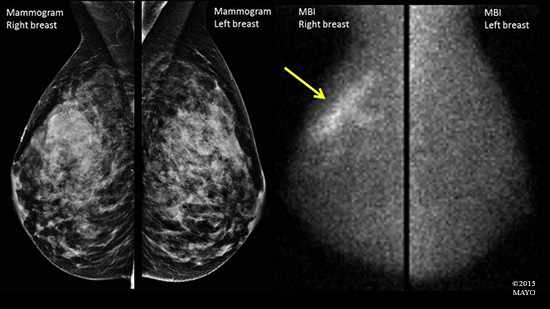
But molecular breast imaging is different than a 3-D mammogram, because it is a functional test ─ not an anatomic test. That means the pictures it creates show differences in tissue activity. Tissue with more active cells, like cancers, light up, or appear brighter, than less active, normal tissue on molecular breast imaging.
Before a molecular breast imaging test starts, you get a small injection of a radioactive tracer into a vein in your arm. The tracer contains a substance that's quickly absorbed by fast-growing cells in the breast, such as cancer cells. Then, a special camera is used to examine the breast. Molecular breast imaging takes about 40 minutes for most women. During the test, your breast is placed in light compression — just enough to hold the breast in place.
When doctors talk about cancers detected by an imaging test, the number is based on how many cancers are found in 1,000 women screened. Molecular breast imaging finds about eight additional cancers per 1,000 women screened, compared to standard mammography. That’s about a 270 percent increase in cancer detection. Tomosynthesis, or 3-D imaging, finds about one to two additional cancers per 1,000 women screened versus a standard mammogram. That’s about a 30 percent increase in cancer detection. Although molecular breast imaging and 3-D mammography have not been compared directly in a controlled study, the numbers suggest that molecular breast imaging detects more breast cancers than 3-D mammography.
But that is not to say that every woman with dense breast tissue must have molecular breast imaging or tomosynthesis. Additional tests can be necessary after either exam, which may not show cancer and be a false alarm. A woman must weigh the chance of needing additional testing and possibly a biopsy that could be normal or benign (not cancer) versus the benefit of possibly finding a cancer not seen on a two-dimensional mammogram.
If you’re unsure of the breast imaging test that would be best for you, discuss the options with your doctor. Together, you can decide on the additional tests that are most appropriate for your situation. — Dr. Katie Hunt, Radiology, Mayo Clinic, Rochester, Minnesota







