-
Featured News
Women’s Wellness: The hysterectomy decision

"The first thing a woman should ask prior to proceeding with a surgical procedure in the form of a hysterectomy is whether there is any other management she can utilize to address whatever issues she’s having," says Dr. Megan Wasson, a Mayo Clinic gynecological surgeon. She says many factors must be considered when deciding to have a hysterectomy. The article below was written by Dr. Wasson for Mayo Clinic's Office of Women's Health.
_______________________________________________________
You need a hysterectomy … what approach is best for you?
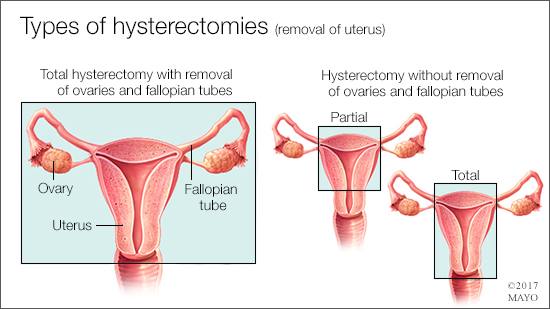
One of the most frequently performed surgical procedures in the U.S. is the hysterectomy. There are many different approaches to completion of this surgery, including vaginal, laparoscopic, robotic and abdominal. Each method has differences that can make it either the right or wrong choice for you.
Important considerations when deciding how your uterus should be removed include why you’re having a hysterectomy, what surgeries you’ve had previously, and if additional procedures will be performed at the time of your hysterectomy. The most important thing to consider when deciding on the route of hysterectomy is how to get the maximum benefit while minimizing your risks.
Friday, Oct. 13, at 5 p.m. CDT
Join a LIVE video Q&A with Dr. Megan Wasson on Mayo Clinic Connect to discuss making the best hysterectomy decision. Learn more about when hysterectomy should be considered, types of hysterectomy, and advantages and disadvantages of different approaches.
Vaginal hysterectomy
During a vaginal hysterectomy, the uterus is removed through the vagina. There are no incisions on your abdomen. Studies have shown that, when possible, vaginal hysterectomy is the preferred approach. This is the most minimally invasive approach and associated with a fast return to normal activities and improved quality of life. When comparing vaginal hysterectomy to laparoscopic hysterectomy, a vaginal approach has a faster surgical time and shorter hospital stay. This is the most cost-effective method and associated with better outcomes. Therefore, the American College of Obstetricians and Gynecologists recommends that whenever feasible, vaginal hysterectomy is the approach of choice.
In order to successfully perform a vaginal hysterectomy, the uterus must be accessible through the vagina. Prior vaginal deliveries or utero-vaginal prolapse increase the likelihood of being able to successfully perform a vaginal hysterectomy. However, if you have not had a prior vaginal delivery or have had previous cesarean deliveries, you may still be a candidate for a vaginal hysterectomy.
Watch: Dr. Wasson discusses the hysterectomy decision.
Journalists: Broadcast-quality sound bites with Dr. Wasson are in the downloads.
Commonly, the ovaries or fallopian tubes need to be removed at the time of hysterectomy. If this is anticipated, having these procedures performed together is not a reason to select an alternative approach to hysterectomy. Removal of the ovaries (oophorectomy) or fallopian tubes (salpingectomy) can easily be performed through the vaginal approach.
If the uterus is noted to be enlarged, morcellation (cutting the uterus into smaller pieces) may be needed. If there is concern for precancerous or cancerous changes in the uterus, vaginal morcellation should not be performed.
Vaginal hysterectomy may not be possible or recommended if you have abnormalities involving the ovaries or fallopian tubes, or severe endometriosis. In these situations, a laparoscopic hysterectomy, with or without robotic assistance, may be better suited. Additionally, cancers involving the ovaries, cervix, or uterus may not be adequately treated with a vaginal hysterectomy. Consultation with a gynecologic oncologist is recommended in these circumstances.
Laparoscopic hysterectomy (with or without robotic assistance)
Performing a hysterectomy through a laparoscopic approach is preferred when a vaginal hysterectomy is not feasible, as this approach continues to have many advantages over abdominal hysterectomy. A laparoscopic hysterectomy requires incisions on the abdomen typically smaller than 1 centimeter. A laparoscopic approach allows for full examination of the abdominal cavity and facilitates excision of endometriosis. If severe endometriosis or pelvic adhesive disease is anticipated, laparoscopic hysterectomy is preferred over vaginal hysterectomy.
If you desire to maintain your cervix, a vaginal approach to hysterectomy is not possible and an alternative approach should be considered. Studies have shown that there are no differences in complications when the cervix is removed or left in place at the time of hysterectomy. Additionally, no clear benefit has been shown in regards to sexual satisfaction and bowel or bladder function. If your cervix is not removed at the time of your hysterectomy, there is still a possibility for development of cervical cancer and you should continue to have Pap smears.
If your uterus is enlarged due to fibroids, it may not be able to be removed in one piece. In this case, the uterus is removed by cutting it into smaller pieces (morcellation). Laparoscopic morcellation of an unexpected cancer has been shown to adversely affect patient outcomes. Therefore, if a cancer is suspected, morcellation should not be performed. However, if the risk of cancer is low, the benefits of a minimally invasive approach to hysterectomy often outweigh the risks.
Abdominal hysterectomy
Abdominal hysterectomy should only be performed when a vaginal, laparoscopic, or robotic approach is not safe or feasible. When compared to vaginal hysterectomy, abdominal hysterectomy has a longer hospital stay, increased pain, and slower return to normal activities. Additionally, when comparing laparoscopic and abdominal approaches, abdominal hysterectomy continues to have a longer hospital stay and slower return to normal activities, but is also associated with more abdominal wound infections and decreased quality of life.
Abdominal hysterectomy is commonly indicated for treatment of gynecologic cancers or when the uterus is significantly enlarged and is unable to be safely removed through a minimally invasive approach.
References
- Committee Opinion No 701: Choosing the Route of Hysterectomy for Benign Disease. Obstet Gynecol 2017;129:e155-e159.
- Tohic AL, Dhainaut C, Yazbeck C, et al. Hysterectomy for benign uterine pathology among women without previous vaginal delivery. Obstet Gynecol 2008;111:829-37.