-
Featured News
Human gut microbe may lead to treatment for multiple sclerosis
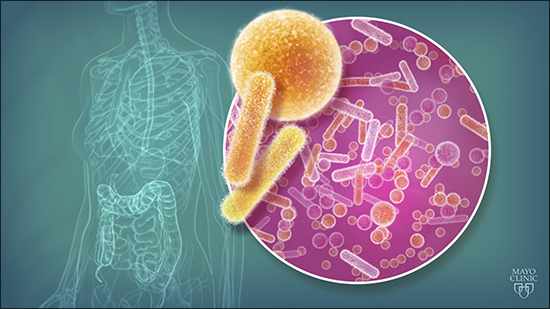
ROCHESTER, Minn. - Mayo Clinic researchers, along with colleagues at the University of Iowa, report that a human gut microbe discovered at Mayo Clinic may help treat autoimmune diseases, such as multiple sclerosis. The findings appear in Cell Reports.
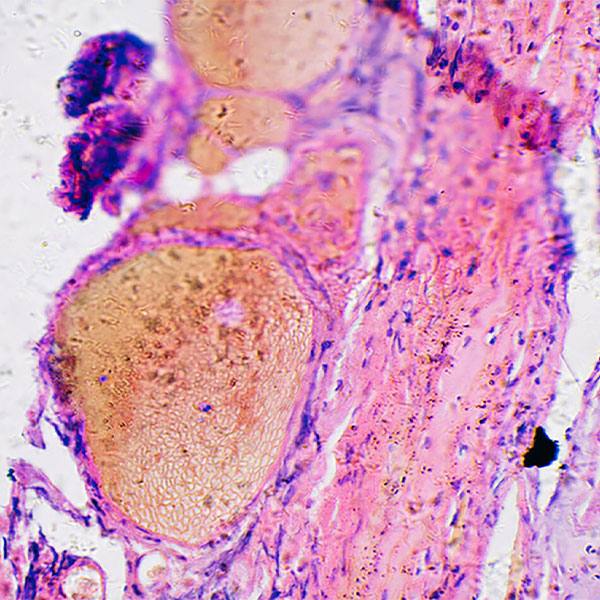
While probiotics have been used for millennia, there are little data showing how a bacterium can provide benefit against a disease outside the gut. This research team tested gut microbial samples from patients on a mouse model of MS. Of three bacterial strains, they discovered that one microbe, Prevotella histicola, effectively suppressed immune disease in the preclinical model of MS.
“This is an early discovery but an avenue that bears further study,” says Joseph Murray, M.D., a Mayo Clinic gastroenterologist and senior author of the article. “If we can use the microbes already in the human body to treat human disease beyond the gut itself, we may be onto a new era of medicine. We are talking about bugs as drugs.” Dr. Murray coined the term “brug” to refer to this approach.
Watch: Dr. Murray discusses the human gut microbe and multiple sclerosiss.
Journalists: Broadcast-quality sound bites with Dr. Murray are in the downloads.
The researchers found that P. histicola, which is cultured from the human intestine, caused a decrease in two types of pro-inflammatory cells, while increasing families of cells that fight disease: T-cells, dendritic cells and a type of macrophage.
The team concludes that, in the future, this type of gut microbe may play a role in treating MS, which is caused by an attack by the immune system on the myelin sheath, a natural insulation that covers the nerves in the brain and spinal cord.
“Our work is a classic example of a bedside to bench and potentially back to bedside study. Recent MS microbiome studies have shown the lack of Prevotella genus in patients with the disease and an increase when patients were treated with disease-modifying drugs,” says Ashutosh Mangalam, Ph.D., first author and assistant professor of pathology at University of Iowa Carver College of Medicine, and principal investigator of the study. “And it’s not just for MS, because this may have a similar modulating effect on other nervous system and autoimmune diseases.”
The research was funded by the U.S. Department of Defense and the National Multiple Sclerosis Society.
Additional authors on the study are:
- David Luckey, Mayo Clinic
- Melissa Karau, Mayo Clinic
- Eric Marietta, Ph.D., Mayo Clinic
- NingLing Luo, Mayo Clinic
- Rok Seon Choung, M.D., Ph.D., Mayo Clinic
- Josephine Ju, Mayo Clinic
- Robin Patel, M.D., Mayo Clinic
- Moses Rodriguez, M.D., Mayo Clinic
- Chella David, Ph.D., Mayo Clinic
- Veena Taneja, Ph.D., Mayo Clinic
- Shailesh Shahi, Ph.D., University of Iowa
- Ramakrishna Sompallae, Ph.D., University of Iowa
- Katherine Gibson-Corely, D.V.M., Ph.D., University of Iowa
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to clinical practice, education and research, providing expert, comprehensive care to everyone who needs healing. For more information, visit mayoclinic.org/about-mayo-clinic or newsnetwork.mayoclinic.org.
MEDIA CONTACTS
Robert Nellis, Mayo Clinic Public Affairs, 507-284 5005, newsbureau@mayo.edu
Molly Rossiter, University of Iowa Health Care, 319-335-8892, molly-rossiter@uiowa.edu