-

Mayo Clinic Researchers Identify Gene that Pushes Normal Pancreas Cells to Change Shape, a Key Step to Cancer Development
JACKSONVILLE, Fla. — A research team led by investigators from Mayo Clinic’s campus in Jacksonville, Florida, and the University of Oslo, Norway, have identified a molecule that pushes normal pancreatic cells to transform their shape, laying the groundwork for development of pancreatic cancer — one of the most difficult tumors to treat.
Their findings, reported in Nature Communications, suggest that inhibiting the gene, protein kinase D1 (PKD1), and its protein could halt progression and spread of this form of pancreatic cancer, and possibly even reverse the transformation.
“As soon as pancreatic cancer develops, it begins to spread, and PKD1 is key to both processes. Given this finding, we are busy developing a PKD1 inhibitor that we can test further,” says the study’s co-lead investigator, Peter Storz, Ph.D., a cancer researcher at Mayo Clinic.
MEDIA CONTACT: Kevin Punsky, Mayo Clinic Public Affairs,
904-953-0746. Email:punsky.kevin@mayo.edu
“We need a new strategy to treat, and possibly prevent, pancreatic cancer. While these are early days, understanding one of the key drivers in this aggressive cancer is a major step in the right direction,” he says.
In the U.S., pancreatic cancer is the fourth most common cause of deaths due to cancer, according to the American Cancer Society. A quarter of patients do not live longer than a year after diagnosis.
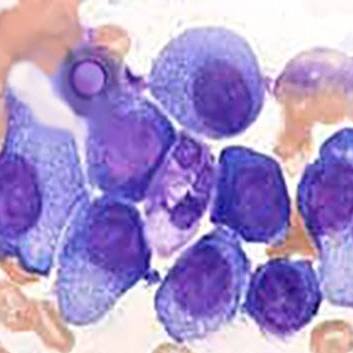
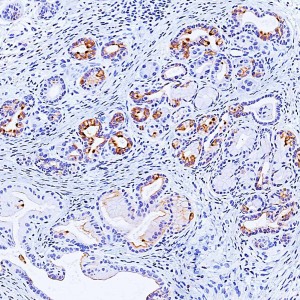
Pancreatic cancer can occur when acinar cells — pancreatic cells that secrete digestive enzymes — morph into duct-like structures. This usually occurs after injury or inflammation of the pancreas and is a reversible process. However, the presence of oncogenic signaling (Kras mutations, EGF-R) can push these duct cells to develop lesions that are at risk for tumor development.
To test PKD1’s effect, the researchers used a 3-D model of pancreatic cells derived from a mouse. They manipulated PKD1 expression by either blocking the gene or inducing its activity. About a week after stimulating PKD1 expression, the researchers could see that acinar cells transformed to duct-like cells. Blocking PKD1 led to decreased formation of duct-like cells and lesions.
“This is a great model for examining what happens in a signaling pathway — we can see the changes by simply using a microscope. This model tells us that PKD1 is essential for the initial transformation from acinar to duct-like cells, which then can become cancerous,” Dr. Storz says. “If we can stop that transformation from happening — or perhaps reverse the process once it occurs — we may be able to block or treat cancer development and its spread.”
The study’s other co-lead investigator is Michael Leitges, Ph.D., of the Biotechnology Centre in Oslo.
Dr. Storz’s work on this study was supported by grants from the American Association for Cancer Research (08-20-25-STOR), the National Institutes of Health (CA135102, GM86435, CA140182) and the Mayo Clinic SPORE for Pancreatic Cancer (P50CA102701).
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to medical research and education, and providing expert, whole-person care to everyone who needs healing. For more information, visit mayoclinic.com or newsnetwork.mayoclinic.org.