-
Cancer
Mayo researchers examine risk factors and patient outcomes associated with colorectal cancer operations, identify benchmarks
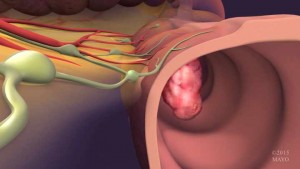 ROCHESTER, Minn. — About 20 percent of colorectal cancer patients have cancers that have spread (metastasized) beyond the colon at the time of their diagnosis. The liver is the most common site for these metastases. The approach to treating primary tumors within the colon and metastatic tumors in the liver continues to evolve; however, it typically involves chemotherapy plus surgical removal (resection) of both types of tumors. However, experts continue to debate whether surgical resection of primary tumors and metastatic tumors should be performed at the same time (synchronously) or in separate operations (sequentially).
ROCHESTER, Minn. — About 20 percent of colorectal cancer patients have cancers that have spread (metastasized) beyond the colon at the time of their diagnosis. The liver is the most common site for these metastases. The approach to treating primary tumors within the colon and metastatic tumors in the liver continues to evolve; however, it typically involves chemotherapy plus surgical removal (resection) of both types of tumors. However, experts continue to debate whether surgical resection of primary tumors and metastatic tumors should be performed at the same time (synchronously) or in separate operations (sequentially).
In the August issue of the Journal of Gastrointestinal Surgery, Mayo Clinic researchers provided a detailed comparison of patient outcomes associated with synchronous and sequential colorectal and liver resections in patients with stage IV colorectal cancer, identifying some benchmarks for surgical practice.
MEDIA CONTACTS: Elizabeth Zimmermann Young, Mayo Clinic Public Affairs, 507-284-5005, newsbureau@mayo.edu
Study findings and conclusions
According to the authors, the study results provide procedure-specific national benchmarks for postsurgical outcomes that will facilitate comparisons for quality improvement. Analyzing data from patients within specific risk categories, the study also yielded these additional findings:
- Major complications after synchronous liver and colorectal resections vary and are related to the extent of liver resection performed and type of colorectal surgery performed.
- The risk for poor patient outcomes increases as the risk of each component surgical procedure increases. In other words, regardless of surgery timing, patients who require higher risk procedures, such as a major liver resection due to the presence of larger or multiple metastatic tumors or high-risk colorectal resections, have poorer outcomes than those who underwent more minor surgery.
- Synchronous resection of primary colorectal tumors and metastatic liver tumors is safe and effective in patients who require only minor liver resections.
“Our findings also show that performing pre-operative risk assessments on patients who require both liver and colorectal resections could allow surgeons to more accurately predict patient outcomes and assist in preoperative planning and counseling these patients,” says David Nagorney, M.D., the article’s lead author and a general surgeon at Mayo Clinic.
Study design and goals
In designing their study, Mayo researchers used a large, multi-institutional database to identify a pool of 43,408 patients who underwent colorectal and liver resections for stage IV colorectal cancer. Before this study was conducted, only limited surgical outcome data was available for these patients.
“Our primary aim was to establish the magnitude of risk that each component operation, both liver and colon, contributed to synchronous resections in order to determine which combination of colon and liver operations were most safe to be performed at the same time,” says Dr. Nagorney.
While past studies had only considered the extent of liver resected performed, Mayo researchers also reviewed the type or location of colorectal resection.
“We wanted to test the hypothesis that both the extent of the liver resection and the location or type of colorectal resection influence the overall risk and patient outcomes associated with these operations,” says the article’s first author, Christopher Shubert, M.D., who is also a surgeon and Kern Scholar at Mayo Clinic.
The researchers assigned risk categories to each of the operations performed in the data pool, including colorectal and liver resections, and then compared 30-day postsurgical outcomes among patients within similar risk groups. They also compared outcome data between two groups of patients within each risk category – those who had synchronous colorectal and liver resections and those who had these operations sequentially.
“Stratifying patients using risk categories allowed us to make more accurate comparisons between patient outcomes associated with synchronous versus sequential resections,” says Dr. Shubert.
This study was made possible in part by the Mayo Clinic Robert D. and Patricia E. Kern Center for the Science of Health Care Delivery and the Surgical Outcomes Program within the center, which is led by study co-authors Elizabeth Habermann, Ph.D., and Robert Cima, M.D. Other co-authors, also from Mayo Clinic, included John Bergquist, M.D.; Cornelius Thiels, D.O.; Kristine Thomsen; Walter Kremers, Ph.D.; and Michael Kendrick, M.D.
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to medical research and education, and providing expert, whole-person care to everyone who needs healing. For more information, visit mayoclinic.com or newsnetwork.mayoclinic.org.







