-
Science Saturday: Designing personalized vaccines to combat cancer
Vaccines have protected people from deadly diseases for generations. Could they also help fight cancer?
Mayo Clinic researchers are working to develop personalized therapeutic cancer vaccines that can potentially target each person's distinctive tumor characteristics. The new approach, built on advances in genomic research and data analytics, holds transformative potential to boost the power of the immune system to identify and attack cancer cells.
"For some patients with cancer, the vaccine may possibly induce their tumors to shrink and provide long-term, durable anti-tumor immunity," says Keith Knutson, Ph.D., co-leader of the Grohne Cancer Immunology and Immunotherapy Program at Mayo Clinic Comprehensive Cancer Center in Florida and co-creator of Mayo Clinic's Neoantigen Personalized Vaccine Program. Dr. Knutson's research is focused on preventing cancer progression.
Dr. Knutson says the individualized cancer vaccines are designed similarly to vaccines for influenza or COVID-19, where the key ingredient is a specific disease-related protein.
"As the immune system learns to recognize that protein, it can stimulate the production of killer T cells to fight it," Dr. Knutson explains.
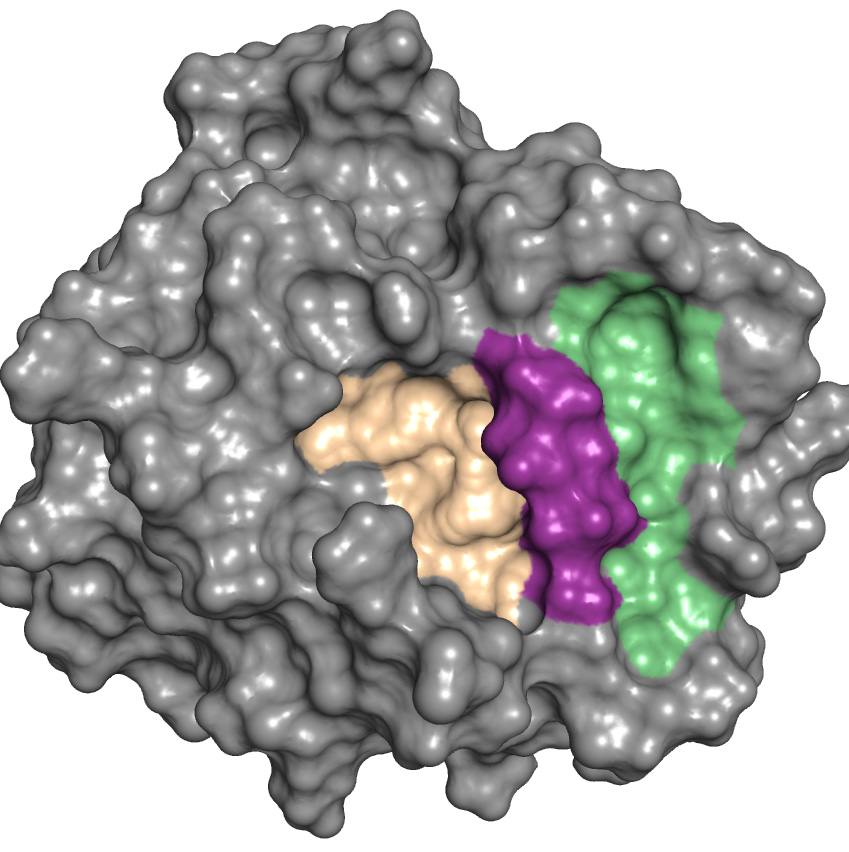
The therapy’s main element consists of bits of a person's unique tumor protein mutations, known as neoantigens. The microscopic protein fragments are generated from gene mutations in tumor cells. Neoantigens are found only on the surface of cancer cells, not on healthy cells.
Because neoantigens are foreign to the body, the immune system can recognize them as pathogenic invaders. When combined with immunotherapy, the vaccine can potentially help generate a robust defensive response.
"The idea is if we can identify between 20 and 30 mutated proteins from a person's cancer, we can formulate those into a vaccine," says Dr. Knutson. "Then we can repeatedly immunize people while they're undergoing treatment with immune checkpoint blockade immunotherapy."
In preclinical animal models, Dr. Knutson and his team delivered the vaccine and immunotherapy combination to treat breast cancer. They found that the dual therapy prolonged survival without causing significant toxicity.
"The hope is that we'll be able to recapitulate those findings in humans," he says.
Designing vaccines for one patient at a time
The vaccine development process begins in Mayo Clinic's Center for Individualized Medicine with sequencing a patient's tumor cells and analyzing the DNA and chains of amino acids — the building blocks of proteins — to find potential neoantigen candidates.
Overseeing the critical selection of neoantigens is Yan Asmann, Ph.D., a bioinformatician at Mayo Clinic in Florida and co-creator of Mayo Clinic's Neoantigen Personalized Vaccine Program. She uses extensive sequencing methods and computational algorithms to choose up to 36 neoantigens — out of hundreds to thousands — that may generate the strongest immune response.
"Some tumors are known to have large changes, like genomic structural rearrangement, where the entire piece of DNA breaks off and fuses back together," Dr. Asmann explains. "Those larger changes actually lead to more foreign neoantigens and are therefore more immunogenic."
Next, Dr. Asmann's team manually validates the quality of each mutation and the accuracy of the neoantigen candidates arising from the mutations.
"We're looking at a massive number of changes in a tumor tissue," Dr. Asmann says. "It's a very complex biological process for neoantigen generation, but it's one that we're working to automate using computational algorithms, including machine learning models."
Once the neoantigens have been selected, Dr. Knutson formulates the vaccine ingredients to enable the strongest possible immune responses for full tumor destruction.
"We then carefully select the neoantigens that can be rapidly manufactured to high purity for safe and timely administration to the patient," Dr. Knutson says.
Dr. Knutson is hopeful the strategy can be introduced into clinical trials soon for the treatment of different types of cancers, as well as for disease prevention.
— Susan Murphy