-

Mayo Clinic Researchers Decode How the Brain Miswires, Possibly Causing ADHD
JACKSONVILLE, Fla. — Neuroscientists at Mayo Clinic in Florida and at Aarhus University in Denmark have shed light on why neurons in the brain’s reward system can be miswired, potentially contributing to disorders such as attention deficit hyperactivity disorder (ADHD).
They say findings from their study, published online today in Neuron, may increase the understanding of underlying causes of ADHD, potentially facilitating the development of more individualized treatment strategies.
The scientists looked at dopaminergic neurons, which regulate pleasure, motivation, reward, and cognition, and have been implicated in development of ADHD.
They uncovered a receptor system that is critical, during embryonic development, for correct wiring of the dopaminergic brain area. But they also discovered that after brain maturation, a cut in the same receptor, SorCS2, produces a two-chain receptor that induces cell death following damage to the peripheral nervous system.
The researchers report that the SorCS2 receptor functions as a molecular switch between apparently opposing effects in proBDNF. ProBDNF is a neuronal growth factor that helps select cells that are most beneficial to the nervous system, while eliminating those that are less favorable in order to create a finely tuned neuronal network.
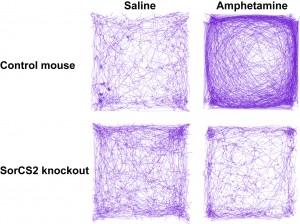
They found that some cells in mice deficient in SorCS2 are unresponsive to proBDNF and have dysfunctional contacts between dopaminergic neurons.
“This miswiring of dopaminergic neurons in mice results in hyperactivity and attention deficits,” says the study’s senior investigator, Anders Nykjaer, M.D., Ph.D., a neuroscientist at Mayo Clinic in Florida and at Aarhus University in Denmark.
“A number of studies have reported that ADHD patients commonly exhibit miswiring in this brain area, accompanied by altered dopaminergic function. We may now have an explanation as to why ADHD risk genes have been linked to regulation of neuronal growth,” he says.
“SorCS2 is produced as a single-chain protein — one long row of amino acids — but it can be cut into two chains to perform a different function. While the single-chain receptor is essential to tell the neuron that it is time to stop growing, the two-chain form tells cells that support neurons in the developing peripheral nervous system to die when they should,” says Dr. Nykjaer.
Unfortunately, if damage occurs to a nerve in the peripheral nervous system, these cells that wrap around and nourish the neurons will die, preventing efficient regeneration, he says. “Our finding suggests that it may be possible to develop drug therapy to prevent this deadly cut of SorCS2 and treat acute nerve injury,” Dr. Nykjaer says.
Other Danish and German researchers contributed to the research. The study was funded by the Lundbeck Foundation and the Danish Medical Research Council.
###
About Mayo Clinic
Recognizing 150 years of serving humanity in 2014, Mayo Clinic is a nonprofit worldwide leader in medical care, research and education for people from all walks of life. For more information, visit 150years.mayoclinic.org, MayoClinic.org or newsnetwork.mayoclinic.org/.
MEDIA CONTACT: Kevin Punsky, Mayo Clinic Public Affairs, 904-953-0746, Email: punsky.kevin@mayo.edu







