Cocaine is like a roller coaster in powder form. First, there is the intense rush of euphoria, excitement, and invincibility. Then, almost as quickly, there is the crash into depression, edginess and cravings for more. A single hit is all it takes, flooding the brain with the feel-good chemical dopamine, subverting the neurons that control learning and reward, and priming the nervous system for the next ride.
It is estimated that 1 in 5 people who try cocaine will become dependent on it at some point in their life. Unlike addiction to opioids, there is no medication to treat addiction to cocaine. The only treatment is abstinence and therapy to help users deal with the relentless cravings that come with it. Relapse is common, and it can be deadly. Among illicit drugs, cocaine ranked as the second or third killer each year between 2010 and 2016.
Now Mayo Clinic researchers are on the cusp of launching a clinical trial that tests gene therapy as a potential treatment for cocaine addiction. The approach employs an enzyme engineered to break down cocaine 1,400 times faster than normal. It inactivates the drug so fast that the user never feels the high, like a thrill-seeker strapping into a roller coaster only to find it transformed into a park bench beneath them.
By taking away the reward associated with drug use, this approach could give hope to the estimated 16 million people addicted to cocaine worldwide.
A Solution in Search of a Problem
"I came to this issue of cocaine abuse in a roundabout way," says Stephen Brimijoin, Ph.D., a Mayo Clinic pharmacologist.
When the Harvard-trained pharmacologist joined Mayo Clinic nearly 50 years ago, he was interested in the biochemical and molecular properties of a family of enzymes called cholinesterases. These enzymes — as the name suggests — catalyze the breakdown of molecules known as choline-based esters, many of which function as neurotransmitters.

Dr. Brimijoin spent years mapping how these molecules help the nervous system work properly, and how they are active participants in neurological disorders such as Alzheimer's disease and dementia. Though cholinesterases are naturally present throughout the animal kingdom, Dr. Brimijoin has explored applications that push the boundaries of what nature intended. His lab has shown how blocking, manipulating and enhancing these ubiquitous enzymes could result in new memory loss treatments, chemical warfare agents and pesticides.
About 20 years ago, Dr. Brimijoin began to consider another application of his favorite enzymes: drug addiction. Butyrylcholinesterase already breaks down cocaine naturally. If the enzyme could be engineered to break down cocaine even faster, he thought it could negate the reward value of the drug.
Dr. Brimijoin turned to Yuan-Ping Pang, Ph.D., director of Mayo Clinic's Computer-Aided Molecular Design Laboratory, to predict which mutations would turn butyrylcholinesterase into a fast metabolizer. They introduced these mutations one after another to generate an enzyme that could inactivate cocaine 40 times faster than normal.
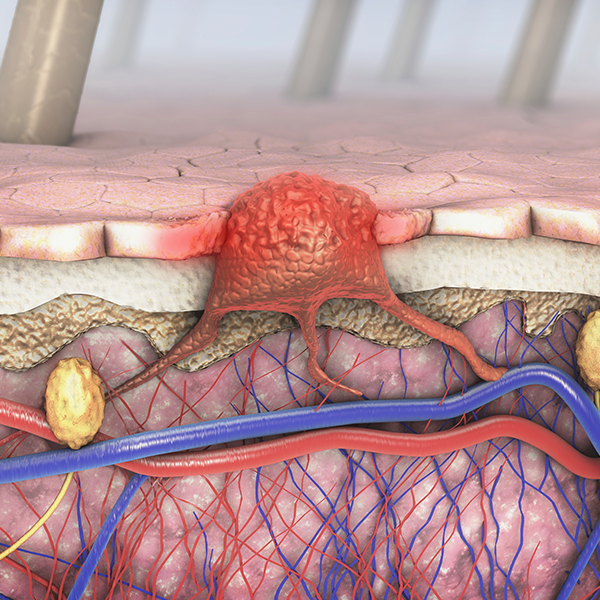
Shortly after they published their results, other researchers discovered several additional mutations that made it work 1,000 times faster and then 1,400 times faster. In a cocaine addict equipped with this enzyme, the drug would be inactivated as soon as it hit the bloodstream, long before it ever reached the brain.

Cutting Cravings
When Dr. Brimijoin and his colleagues tested the new enzyme in mice, the results were startling. The mice treated with the enzyme were able to tolerate doses of cocaine that normally would induce massive convulsions followed by death within minutes. Though pleased, Dr. Brimijoin worried that the increased tolerance was not enough. It was one thing to survive a lethal dose of cocaine. It was quite another to survive the cravings that resulted after the drug was taken away.
"It is the craving that is overwhelming, leaving people basically helpless," says Dr. Brimijoin. "We needed a delivery system that would extend its activity for at least months or a couple of years, though perhaps not forever. Gene therapy seemed like the answer."
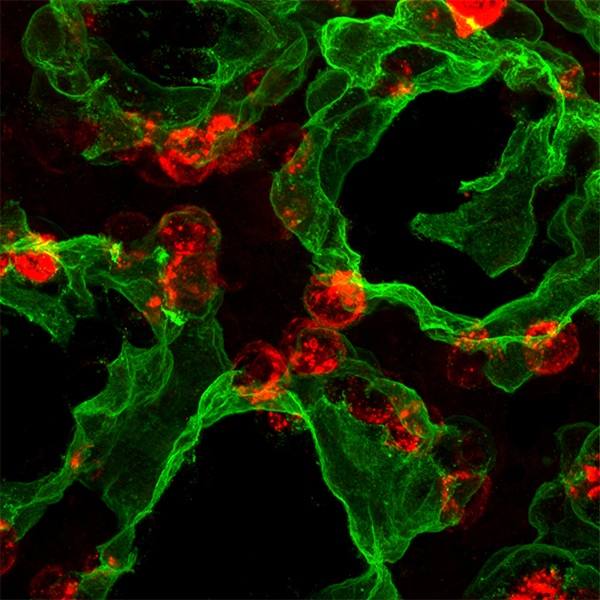
This time, he worked with Liyi Geng, Ph.D., a senior research technologist, to design a viral delivery system (viral vector) to get the genetic material for the supercharged enzyme into cells. They packaged the gene for butyrylcholinesterase into adeno-associated virus, or AAV, a relatively harmless carrier that is already present in most of the human population. The virus has been used to safely deliver gene therapy in clinical trials for several diseases, including eye disease, congestive heart failure, Parkinson's disease, and muscular dystrophy.
The researchers injected mice that had been trained to abuse cocaine with a single dose of this vector or a similar dose of saline. While the mice that received a dose of saline kept pushing the lever to self-administer cocaine, the ones that got the enzyme stopped asking for more hits of the drug. "They behaved as if they didn't care about it anymore," says Dr. Brimijoin. "It was as if their cravings were gone."
Unforeseen Benefits
Before attempting a move to human studies, the researchers decided to follow treated and untreated mice for years to see if there were any toxic effects of the gene therapy. They kept several cages in the animal care facility, with five male mice to a cage. Within a few months, Dr. Brimijoin received a call from the facility that the mice in cage No. 3 were fighting and needed to be separated. The next week brought another call about another cage, and then another.
After a while, he realized that all the calls were about the untreated, cocaine-addicted mice — not the ones that received gene therapy. When he sent scientists from his lab to visit the facility, they witnessed the treated mice playing with each other, running around in their cage and having fun.
"I thought, what the heck is going on?" says Dr. Brimijoin. "So I invoked a powerful approach: Google." When he entered "butyrylcholinesterase" and "stress hormone," up popped the term "ghrelin," an infamous hunger hormone.

Back at the bench, his team found that the treated mice had drastically low levels of ghrelin in their bloodstream. "It was a hall of mirrors," Dr. Brimijoin says. "Nothing was the way we thought it should be." But after a series of experiments, he and his team began to make sense of their findings.
They found that butyrylcholinesterase was drastically lowering ghrelin levels in the general circulation and preventing the hormone from reaching the brain. In turn, the receptors in the brain involved in tamping down cravings became particularly sensitive. As a result, the mice no longer craved cocaine. Rather than craving another hit, they just wanted to play.
The Sky's the Limit
Thus far, the researchers have used gene therapy to curb cocaine cravings in successive animal models. Recently, Dr. Brimijoin has partnered with W. Michael Hooten, M.D., a Mayo Clinic anesthesiologist, to lay the groundwork for taking the approach into humans.
"Having this type of therapy could literally revolutionize treatment of life-threatening addiction," says Dr. Hooten.

For now, the researchers are continuing to assess the possible toxicity of the gene therapy. With a $1.35 million grant from the National Institute of Drug Abuse, they acquired preclinical data that led to an investigational new drug permit from the Food and Drug Administration. The remaining major obstacle to clinical trials is the preparation of clinical-grade vector at the Children's Hospital of Philadelphia.
Dr. Hooten believes that if all goes well, the treatment potential is tremendous.
"The majority of drugs that are really problematic are associated with high levels of drug craving, whether it's alcohol, opioids, cocaine, methamphetamine or nicotine," says Dr. Hooten. "If this treatment truly reduces cravings, it could potentially disable the addictive power of illicit drugs."
It is possible that one day roller coasters may be the only way to get high.
— Marla Vacek Broadfoot, Ph.D.