-
Featured News
Mayo Clinic Q and A: Patient Should Talk to Doctor About Interest in Discontinuing Anti-Epileptic Medication
DEAR MAYO CLINIC: I was diagnosed with epilepsy three years ago at the age of 29. I’ve been on medication since then and haven’t had another seizure. Is it true that, for some people, epilepsy is not necessarily a lifelong condition? Is there a way to determine if I can safely go off of the medication to see if I need it anymore?
ANSWER: Medication often can control epilepsy effectively and eliminate seizures. In a case like yours, where you’ve been seizure-free for several years, it may be reasonable to consider discontinuing anti-epileptic medication. However, the decision about the duration of your therapy needs to be made by your physician after careful consideration of how likely it is that you may have seizures again.
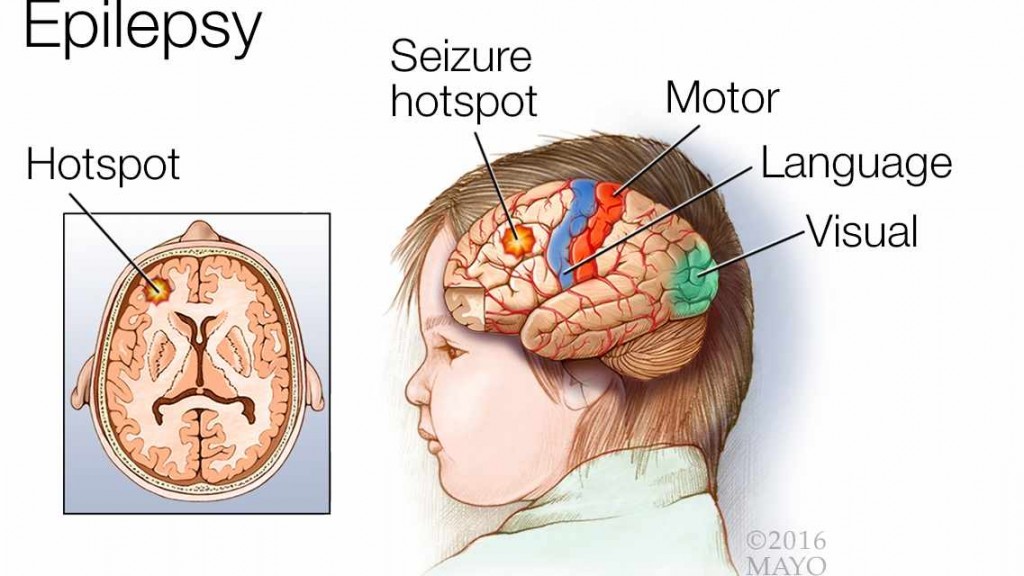
Epilepsy is a central nervous system disorder. In a person with epilepsy, nerve cell activity in the brain becomes disrupted, causing seizures or periods of unusual behavior, sensations and, sometimes, loss of consciousness. The symptoms of a seizure can vary widely from one person to the next. For example, some people with epilepsy stare blankly for a few seconds during a seizure or appear confused. Others may lose consciousness and have repetitive jerking of their arms and legs.
About 10 percent of people in the U.S. have a single, unprovoked seizure at some point in their lives. Having one seizure, however, doesn’t mean you have epilepsy. At least two unprovoked seizures generally are required for an epilepsy diagnosis. Epilepsy may be associated with a neurologic disorder, such as a stroke, tumor or head trauma. But, in many cases, a specific cause of seizures cannot be identified.
Even mild epilepsy requires treatment, because seizures can be dangerous during activities such as driving or swimming. As in your case, medication to reduce or eliminate seizures usually is the first step in treatment. For many people, that’s all they need to keep seizures in check. A variety of anti-epileptic drugs are available. Doctors take into consideration your condition, medical history, how often you have seizures, your age and other medication you take, among other factors, when choosing which anti-epileptic medication to prescribe.
It may take several tries to find the right medication and dosage to control seizures. About two-thirds of patients have their seizures effectively controlled with either the first or second drug they use. It’s not uncommon for people to be seizure-free from that point on. Eventually, more than half of children with epilepsy who aren’t experiencing symptoms can discontinue medications and go on to live a seizure-free life. Many adults also can discontinue medications after two or more years without seizures.
To help decide if discontinuing medication is a good choice for you, your doctor should carefully review your overall medical history, as well as your history of seizures. If your seizures were mild and infrequent before you began taking anti-epileptic drugs, it may be more likely that you will not have additional seizures when you stop taking the medication.
Your doctor also may suggest several tests to assess your condition before you stop taking medication. These could include an electroencephalogram, or EEG, to check the electrical activity in your brain. Depending on your situation, an MRI of your head may be helpful, too, if you have not had one in the past. If your doctor does recommend you stop taking anti-epileptic medication, and you remain seizure-free, you still may need follow-up appointments from time to time to check your condition.
It’s important to note that anti-epileptic medications usually aren’t suddenly discontinued. That could provoke seizures. In most cases, doctors prescribe a tapering of anti-epileptic drugs, which involves a gradual withdrawal over several weeks.
Make an appointment to talk with your doctor about your interest in discontinuing medication. From your description, it sounds like your situation is one in which that could be a realistic option. — Dr. Gregory Cascino, Neurology, Mayo Clinic, Rochester, Minnesota