Neurosciences
April 29, 2024
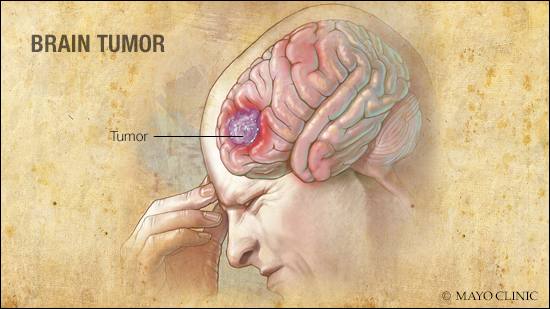
DEAR MAYO CLINIC: I have been diagnosed with a brain tumor and advised to have radiation therapy. I'm very nervous about this and the risks[...]
March 2, 2013
February 27, 2013
February 21, 2013
January 25, 2013
January 10, 2013
December 10, 2012
December 5, 2012
Explore more topics
 Sign up
Sign up

Mayo Clinic Connect
An online patient support community
