-
Research
A Mayo Clinic collaboration studies engineered stem cells for liver disease
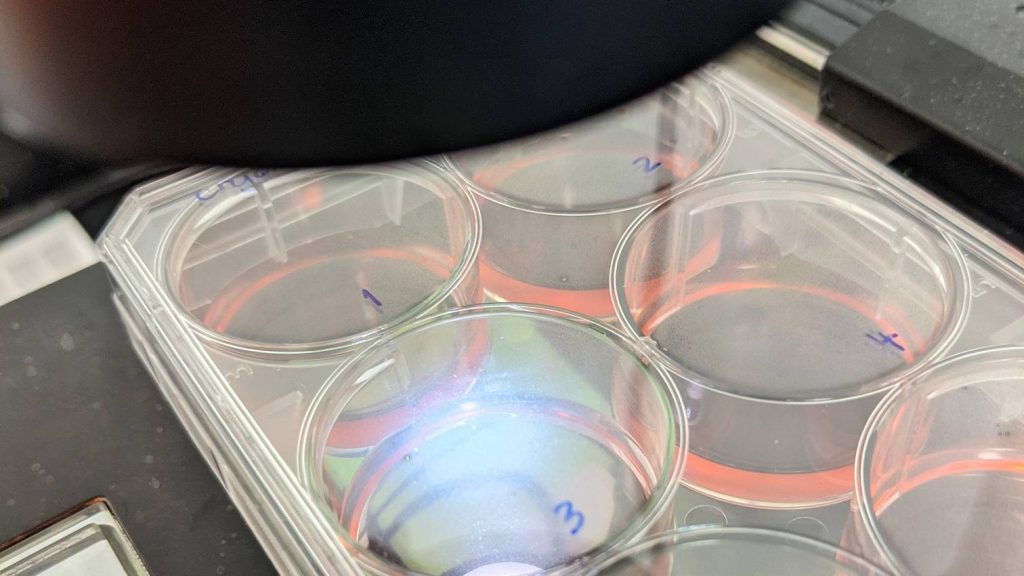
Mayo Clinic's Center for Regenerative Biotherapeutics is collaborating with the biotech firm HepaTx on an experimental therapy to regenerate tissue in patients with late-stage liver disease. This new technology takes mesenchymal stem cells from adipose (fat) tissue and coaxes them to function like hepatocyte (liver) cells. The purpose of the collaboration is to move this technology to early clinical trials and study its effect on people with liver damage from alcohol-related hepatitis.
Mesenchymal stem cells are adult stem cells that have been well studied and have been shown to be safe in humans.
Mayo Clinic brings to the collaboration expertise in regulatory affairs, clinical trials, product development and biomanufacturing. HepaTx brings a new cell technology directed toward a disease with few therapeutic options. Together they will work to advance the engineered liver cells to first-in-human safety studies.

"Our goal in working with industry is to quickly bring a pipeline of cell-based therapeutics to patients with unmet needs," says Julie Allickson, Ph.D., chief technology officer at Mayo Clinic's Center for Regenerative Biotherapeutics. "This is a very exciting opportunity to pair Mayo Clinic's know-how with a new discovery aimed at improving the health, lives and therapeutic outcomes for patients."
A new cell-based therapy for liver disease
Excessive alcohol use damages and eventually destroys liver cells, causing inflammation that can lead to abdominal pain, scarring and liver failure. Alcoholic hepatitis is one type of chronic liver disease that affects 20-40% of heavy drinkers.

In the early stage of liver disease, treatment is aimed at managing the symptoms through a combination of small molecule drugs and quitting drinking. However, in later stages, cell and tissue damage are often irreversible. People with end-stage liver disease may need an organ transplant to survive.
The engineered liver cell technology from HepaTx is so new that it has never been manufactured on a large scale for patients. That's where the Center for Regenerative Biotherapeutics process development experts come in. They develop standard operating procedures —a blueprint of sorts — for biomanufacturing in Mayo Clinic's state-of-the-art current Good Manufacturing Practice (cGMP) facilities. CGMP refers to a set of practices that ensures a new therapy meets strict quality control and quality assurance standards for medicines made from living sources such as cells.
"We engage with investigators at proof of concept. We guide the technology through process development to identify any gaps in safety that could delay regulatory approval for a clinical trial," says Dr. Allickson. "Our biomanufacturing infrastructure is based on industry best practices, which positions us well to work with outside collaborators to advance a new therapy toward market approval for patients."
Mayo Clinic will lead the early clinical trials in which patients with alcohol-related hepatitis will be infused with the engineered liver cells. The research will focus on safety and effectiveness of this cell replacement therapy in repairing late stage disease.
Working with industry collaborators that are aligned with Mayo Clinic values is a strategic priority for the Center for Regenerative Biotherapeutics.
Mayo Clinic has a financial interest in the technology referenced in this article. Mayo Clinic will use any revenue it receives to support its not-for-profit mission in patient care, education and research.
###
Related stories:
Mayo Clinic secures ARPA-H award to build a living pharmacy within the body for inflammatory disease
Innovation centers spur new biotherapeutics for patients







