-

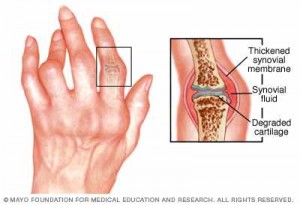
Blood Test Could Prevent Medication Trial and Error for Rheumatoid Arthritis Patients
Boston — A molecule in the blood shows promise as a marker to predict whether individual rheumatoid arthritis patients are likely to benefit from biologic medications or other drugs should be tried, a Mayo Clinic-led study shows. The protein, analyzed in blood tests, may help avoid trial and error with medications, sparing patients treatment delays and unnecessary side effects and expense. The research is among several Mayo Clinic studies presented at the American College of Rheumatology annual meeting in Boston.
Researchers tested blood samples taken before rheumatoid arthritis treatment was given. The patients then were treated with anti-inflammatory biologic drugs, tumor necrosis factor-alpha inhibitors, a new class of medications used for rheumatoid arthritis. They found that a protein made by the immune system, type 1 interferon, appears to serve as a valid marker to tell whether individual rheumatoid arthritis patients will respond to biologics, or other medications should be tried.
MEDIA CONTACT: Sharon Theimer, Mayo Clinic Public Affairs, 507-284-5005, Email: newsbureau@mayo.edu
Journalists: Sound bites of Dr. Niewold are available in the downloads below.
“We are trying to personalize therapy for rheumatoid arthritis. One of the main problems rheumatologists have had is that it’s hard to choose the right drug for the right person,” says senior author Timothy Niewold, M.D., a rheumatologist at Mayo Clinic in Rochester, Minn.
“Each new drug works for some people and not others. It’s not trivial, because the disease causes damage in the joints and if it takes a year or two to find the right treatment, then damage can accrue,” Dr. Niewold says. “In the study, we looked at markers in the immune system that might help us guide our treatment choices.”
Methotrexate is often the first drug tried for rheumatoid arthritis. If that doesn’t work, biologics are often next. Those carry side effects including risk of infection, and people should be tested for tuberculosis before taking them.
Getting rheumatoid arthritis under control is important not only to prevent the damage it causes directly, but to reduce the risk of other serious conditions, such as heart disease. Rheumatoid arthritis patients are twice as likely to develop heart disease as the average person, and previous Mayo research has found that the severity of the rheumatoid arthritis is a factor. People for whom methotrexate doesn’t work tend to have more severe rheumatoid arthritis, Dr. Niewold noted.
More research is needed before use of the marker becomes standard practice, Dr. Niewold says. A larger trial involving several institutions is under way. Future studies may examine whether the marker can also help guide medication decisions for other conditions treated with biologics, such as psoriatic arthritis, psoriasis and inflammatory bowel disease, he says.
In other studies being presented at the American College of Rheumatology meeting, researchers found:
- Rheumatoid arthritis patients and their physicians often describe pain differently, leading to a gap between what patients understand their pain levels to be and how physicians rate the pain. Patients are more likely to describe pain using words with emotional connotations, possibly reflecting the activation of pain, mood and fear networks in the brain by inflammation, the researchers say. Physicians, meanwhile, are likelier to use sensory descriptions such as “sharp, aching or throbbing” to characterize pain. Further research can help physicians develop new approaches to better ease pain, the study authors say.
- Rheumatoid arthritis flare-ups raise patients’ heart disease risk. “Every time joints flare up, it’s a knock against their hearts,” says co-author Eric Matteson, M.D., rheumatology chair at Mayo Clinic in Rochester. “Patients should keep track of their flare-ups and call their physician when they have a flare.”
- Like people with rheumatoid arthritis, those with psoriatic arthritis are at higher risk of cardiovascular disease. Heart disease prevention, detection and treatment efforts are especially important for such patients, the researchers say.
- Rheumatoid arthritis patients, whether women or men, are likelier to be hospitalized than people without the inflammatory disorder. Men with rheumatoid arthritis are likelier to be hospitalized for depression, while women and people 45 to 64 with rheumatoid arthritis are likelier to be hospitalized for diabetes.
The Rheumatology Research Foundation and National Institutes of Health provided funding for the type 1 interferon study.
Financial disclosures:
- Dr. Niewold: Janssen Pharmaceutica Products, LP; EMD Serono; Biogen Idec.
- Hilal Maradit Kremers, M.D., of Mayo Clinic, a co-author of the psoriatic arthritis study:
- Rheumatoid arthritis flare study co-authors Elena Myasoedova, M.D., Ph.D., Arun Chandran, M.B.B.S., Cynthia Crowson and Brittny Major of Mayo Clinic: Roche Pharmaceuticals.
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to medical research and education, and providing expert, whole-person care to everyone who needs healing. For more information, visit http://www.mayoclinic.org/about-mayo-clinic or https://newsnetwork.mayoclinic.org/.