-
Discovery’s Edge: Tackling Polycystic Kidney Disease
The term "teamwork" is widely used when talking about scientific research, but when it comes to the Mayo Clinic version, it means cross-disciplinary teams with complementary members. Some teams form to pursue special problems for limited periods, while others form alliances that last for years, with prolific results. The latter is the case with a physician-researcher and a lab scientist, one older and accomplished, the other younger with new ideas and needed skills. Together they are tackling some of the toughest problems in kidney disease.
Even if you're tops in your field, you may need a partner with skills you don't have.
That was the conclusion Mayo Clinic nephrologist Vicente E. Torres, M.D., Ph.D., came to about 15 years ago. As part of Mayo Clinic's Division of Nephrology and Hypertension in Rochester, Minnesota, he had worked at Mayo Clinic nearly a quarter century and was renowned as a physician and researcher who specialized in polycystic kidney disease (PKD).
As the importance of genetics in human diseases — especially PKD — became ever more obvious, Dr. Torres knew he needed help. He needed someone who could understand the cause of disease at the molecular level.
"Medicine entered a new phase where genetics became really very important, not only for monogenic diseases like polycystic kidney disease, but for almost all diseases that have a genetic component," Dr. Torres says. "In nephrology at that time, we really didn't have anyone who was trained in molecular genetics. So I thought that it was a very good idea to try to attract people like that here to Mayo."
He recruited Peter C. Harris, Ph.D., a molecular geneticist from the University of Oxford whom he knew from international conferences and meetings. At the Institute of Molecular Medicine in Oxford, Dr. Harris headed the team that had identified the gene that causes the most common form of polycystic kidney disease. Dr. Harris arrived at Mayo Clinic in Rochester, Minnesota, in 1999, launching a partnership that has probably worked better than either investigator imagined it could.
Complementing medicine with science
Drs. Torres and Harris have coauthored dozens of scientific papers and have published scores of other studies individually or with other collaborators. Their research on PKD has led to new understanding of the disease, its causes and its progression, and today, the possibility of new treatment options.
"What you have in that combination is one of the best examples of a clinician-scientist teaming up with a basic scientist, bringing their own and complementary tools and expertise in the hope there will be new and better treatments," says Karl A. Nath, M.B.,Ch.B., a Mayo Clinic nephrologist in Rochester. "There's no redundancy. It's an instance of one and one makes four rather than two."
Despite their close collaboration, the two scientists are a study in contrasts. Dr. Torres, the older of the pair, is professorial in his salt-and-pepper beard, his speech serious and measured, with a trace of a Spanish accent. In contrast, Dr. Harris seems like an English schoolboy with a droll sense of humor. He jokes that Dr. Torres lured him to visit Minnesota in the middle of one of the warmest winters on record, as though Harris had no idea what was in store for him.
"I think it was 40 degrees when we were here," Dr. Harris says. "It certainly wasn't like that last winter."
Not surprisingly, the two scientists came to specialize in PKD in entirely different ways. For Dr. Torres, it was a matter of public health. He was already a nephrologist at Mayo Clinic when he had the opportunity to examine the prevalence and outcomes of polycystic kidney disease in Olmsted County, the southeastern Minnesota county that includes Mayo Clinic.
"I found polycystic kidney disease to be a fascinating field," Dr. Torres says. "To get the understanding of how the kidney works and how the kidney fails in polycystic kidney disease, there are also other organs and systems involved — the liver, the heart and the vascular system."
For Dr. Harris, on the other hand, it was all about genetics.
"I was very interested in how we could use the new genetic methods — the identification of polymorphic markers," he recalls. "It's rudimentary now, but it seemed cutting edge at the time."
Genetic, chronic and complex kidney disease
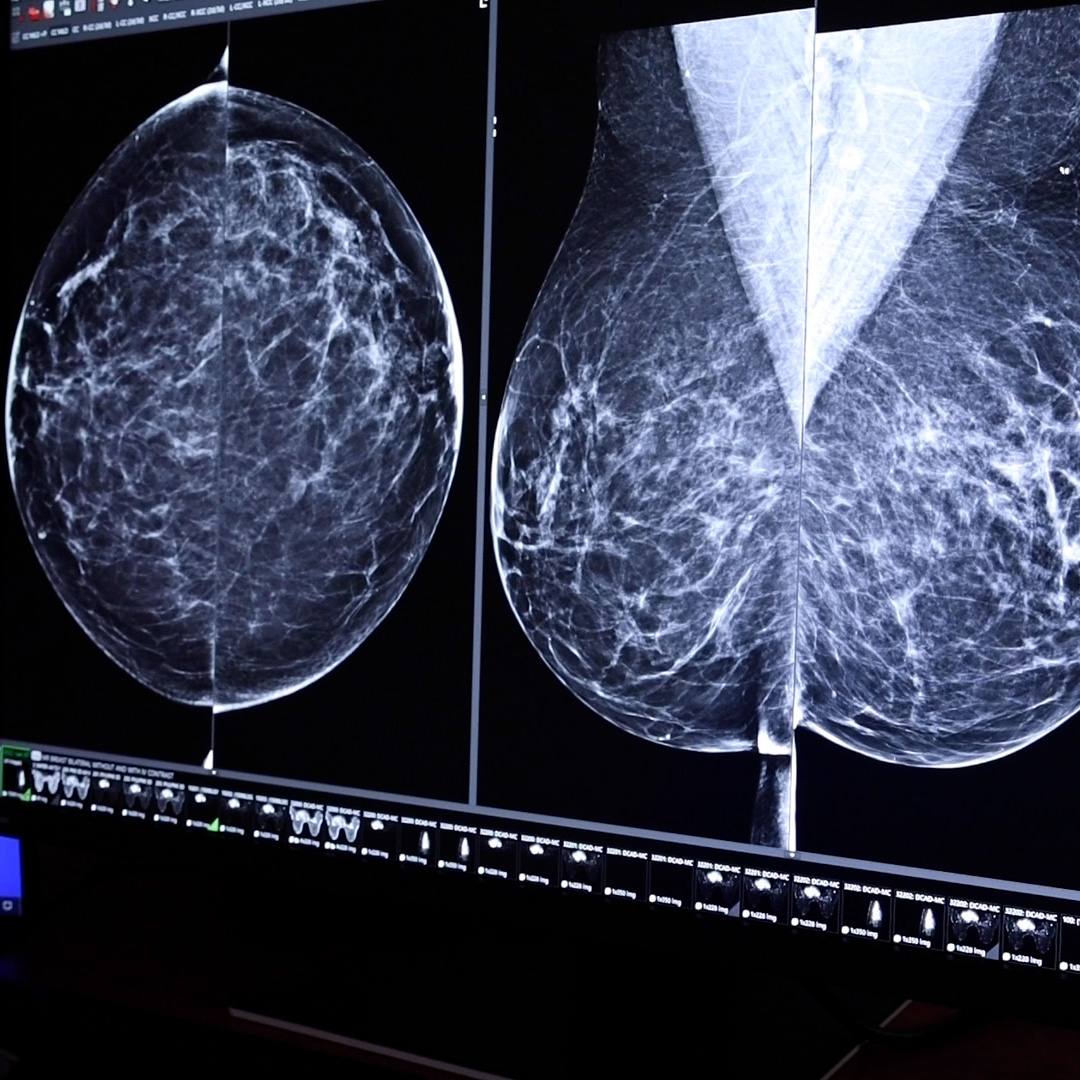
The impact of the multiple cysts of PKD compared to a healthy kidney.
Polycystic kidney disease is an inherited disorder that develops as clusters of cysts grow within the kidneys or other parts of the body, typically causing high blood pressure and kidney failure.

Although it's a genetic disorder, children aren't routinely screened for PKD. Dr. Torres does recommend screening adults with a family history of the disease.
There are actually two types of PKD, each caused by a different genetic flaw. Autosomal dominant PKD, the most common type of polycystic kidney disease, is caused by an abnormality in one of two genes. A child with one affected parent has a 50 percent chance of developing PKD. Signs and symptoms usually start developing around ages 30 to 40. Far less common is autosomal recessive PKD, in which both parents must have the genetic abnormality to pass the disease to their children. In this form of PKD, abnormalities in kidney and liver function show up in infancy or childhood. Many children with autosomal recessive PKD die in infancy. Those who survive often develop high blood pressure and need a kidney transplant in childhood.
At the core of PKD, Dr. Torres says, are the 1 million filters and tubules that make up each kidney.
"When these genes don't work properly, these tubules don't know when to stop growing and form the cysts," Dr. Torres explains. "As they grow, they destroy the tissue. The kidney gradually loses its function."
According to the National Institutes of Health, about half the patients with the dominant form of PKD have end-stage renal disease by age 60, and every year in the United States more than 2,000 begin kidney replacement therapy, such as transplant or dialysis.
Seeking treatment answers
Most patients with PKD receive treatment for high blood pressure and pain. They may control cholesterol and are screened for brain aneurysms. Otherwise, there's little to be done until kidneys fail and a transplant becomes necessary.
"If we can slow down or stop the progression in these patients, then we can alleviate some of the problems by delaying renal failure, transplantation or dialysis," Dr. Harris says. "Obviously, we'd like to completely cure the disease, but even if we could slow it down or slow down the progression of the disease by five or 10 years, that would be a big breakthrough."
Dr. Harris examines downstream signaling effects — how genes, such as the abnormal PKD gene, create various molecules that signal, or stimulate, cell membrane receptors and affect the formation of tubules in the kidney. To conduct these experiments, Dr. Harris engineers a variety of mice and zebrafish in which specific genes are removed or changed. The results from these experiments were published in 2014 in the American Journal of Physiology — Renal Physiology and the Journal of the American Society of Nephrology.
"Making the right mouse, one that really matches the way that the disease progresses in humans — or speeding it up a little bit, so you don't have to wait 50 years — has been something we've spent quite a lot of time on," Dr. Harris says. The trick is to mimic the onset of the disease fast enough to be efficient but slowly enough to keep the animal alive for study.
Dr. Torres' work picks up where Dr. Harris' leaves off. He spends a quarter of his time seeing patients and the remainder in PKD research. That includes characterizing the progression of the disease and developing clinical trials for potential new medications and other therapies. One important result of their collaboration: The discovery of a compound that inhibits the signaling of a particular molecule and slows by half the progression of PKD. This discovery was published in the New England Journal of Medicine in 2012. Using the compound in treatment for patients has been approved in Japan but has not yet been approved for use in the United States.
Meanwhile, says Dr. Torres, "There are a lot of candidate drugs that need to be tested — more that need to be tested than there is money available for clinical trials."
In addition to new drug discoveries, another priority is developing new imaging technologies to examine the progression of polycystic kidney disease long before symptoms appear.
"If you want to treat, you have to be able to measure," Dr. Torres explains. "So to be able to measure before the kidney function goes down is something that is very important."
Other work focuses on preventing the passage of PKD to the next generation. Mayo Clinic has begun providing preimplantation genetic diagnosis for PKD, in which doctors screen out embryos that carry the gene for PKD before implantation and pregnancy. In the future, Dr. Harris says, the two researchers hope to find other genetic factors that influence the severity and progression of polycystic kidney disease. Eventually, gene editing may be possible.
"You can imagine that potentially you might be able to gene-edit at a very early stage," he says. "Those cells would go back and populate the embryo. It's looking more promising than it did even a couple of years ago."
Better patient care found in team science
The collaboration between Drs. Torres and Harris has created a synergy that has allowed them to make major strides in the understanding and treatment of PKD. What makes this such a fruitful collaboration between a basic scientist and a clinician?
Partly, it's environment. Mayo Clinic's tightly knit campus helps.
"Here you have a lot of physicians from the clinic and researchers working side by side," Dr. Harris says. "Everything and everyone is just three or four minutes away."
And it helps that in this collegial setting a culture of collaboration has developed, says Dr. Torres. He and Dr. Harris have conducted studies along with liver specialists and surgeons, neurologists and vascular surgeons, kidney radiologists, and vascular radiologists.
"I think all of these people are top in their areas, so having the ability to collaborate with these people is something that Mayo brings," he says.
"If you're both trying to do the same thing, it doesn't really work out well," Dr. Harris says. "When you have different expertise and you can put it in and enhance the final product, which is what we've been doing, I think that's when collaboration really works — when you can make a much better product than either of us could make individually."
-- Greg Breining
September 2015