June marks the 40th anniversary of the first scientific report describing pneumocystis pneumonia, which later became known as acquired immune deficiency syndrome (AIDS). More than 32 million people have died worldwide from AIDS and 38 million people are living with HIV, the virus that causes AIDS, according to the Centers for Disease Control and Prevention.
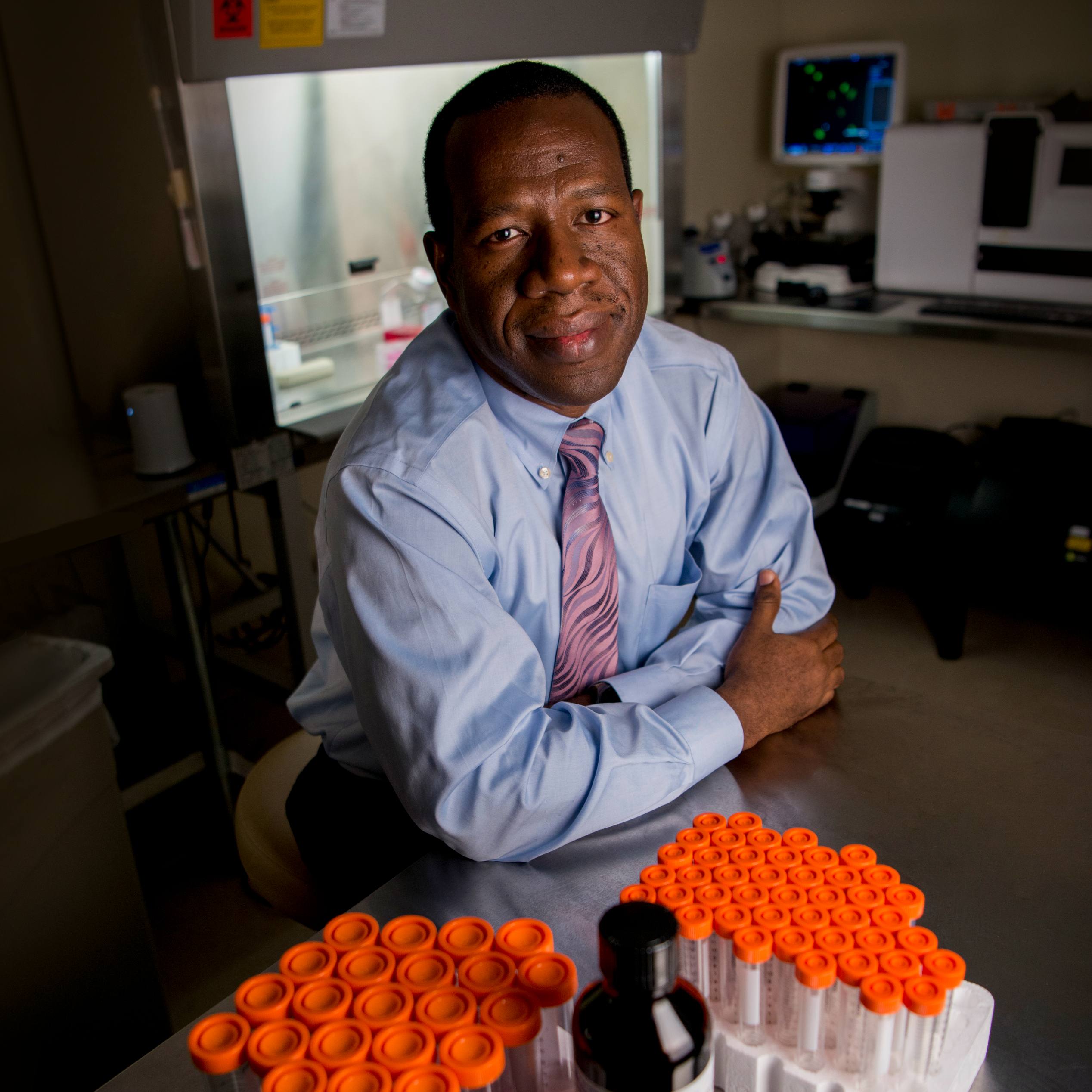
"The last 40 years of the HIV epidemic have given us an in-depth look at society, science, medicine, and socioeconomic impacts of disease on communities and countries. Forty years ago was the very first report. Still, we didn't even know what the causative agent was," says Dr. Stacey Rizza, a Mayo Clinic infectious diseases physician and HIV researcher.
Unfortunately, the AIDS crisis of the 1980s was steeped in misinformation and discrimination, especially against gay men who were disproportionately affected by the disease. Much progress has been made since that time, but there is still more work to be done.
"Being diagnosed with HIV/AIDS has a different meaning than it did just two decades ago, says Dr. Rizza. "It’s a whole new world, and, for those of us who are a little older and started treating HIV in the ‘90s and saw that world, it was tragic. We watched wonderful people who were brave and fought their virus but unfortunately, we weren’t able to stop the virus from replicating."
HIV is a sexually transmitted infection spread through contact with infected blood, semen or vaginal fluids. The virus also can be spread by sharing drug needles and syringes, and less commonly from mother to child.
Watch: Dr. Stacey Rizza talks about 40 years of HIV/AIDS research.
Journalists: Broadcast-quality sound bites with Dr. Rizza are in the downloads at the end of the post. Please courtesy "Stacey Rizza, M.D. / Infectious Diseases / Mayo Clinic."
In this Q&A, Dr. Rizza provides some insight to understand the research and why AIDS is such a difficult disease to cure:
What did the early research find?
Because of truly dedicated innovative science, within a few years, the scientific community figured out that AIDS was due to HIV. It then took a few years to figure out how to test for that virus. Several years later, the scientific community was able to quantitate how much virus was in a person's blood. During all this time, truly innovative research into how the virus replicates and how the immune system responds to the virus allowed bio pharmacy companies to develop what we call anti-retroviral drugs or medications to slow down the viral replication.
How has medication to treat HIV evolved?
The first drug approved for HIV was in 1987, which was AZT (now known as zidovudine). At that time, it was the fastest drug ever approved by the FDA (Food and Drug Administration) and started the fast-track mechanism through the FDA.
Then several other drugs within that same class were approved in the early 1990s. In late 1995, very early 1996, the first HIV protease inhibitors were approved. At that point, it was possible to combine three different medications from two different classes and completely suppress the HIV replication.
In the last 20 years, we've gone from people taking multiple medicines with lots of side effects to many of my patients with HIV now take a single pill a day. That's a combination of medicines coformulated into one pill a day that's extremely well-tolerated and completely suppresses their virus. We know it does not eliminate the virus. If they were to stop taking that medicine, the virus would come back. But we now have a handful of people in the world who have been what we called functionally cured of HIV, meaning they've gone through some research protocols that eliminated the reservoir of HIV in their body.
The new drugs are so effective in people who have fully suppressed virus that many only need to use two medications to maintain HIV treatment and control. New research is investigating ways to deliver the medications differently, such as a shot that lasts several months, or maybe someday even implantable medication delivery mechanisms so that people don’t have to take the pill every day. It is very exciting that HIV therapy is moving that direction.
Why isn't there a cure for HIV?
The reason why it is so difficult to cure HIV is that once HIV infects a person's body, it integrates into the host genome of several cell types. Those cells then hide in any of the lymphoid tissue, such as the lymph nodes, the liver and the spleen. And they lay there as what we call "latent" or "hiding", as long as the person is on HIV therapy. Anytime a virus does leave a cell, it gets taken care of by HIV therapy. But if the infected individual stops the HIV therapy, that latent virus will come back. To cure HIV, you have to eliminate those hiding viruses in the cells or that latent viral reservoir, which is the term. There are many ways you can approach eliminating the reservoir.
Where is the research now?
One of the more popular ways that have been investigated is something called — and there are many different terms for it — “prime, shock, and kill” or “kick, and kill”, which is essentially giving medications that first wake the virus up from latency and then find ways to make the cells that have the virus susceptible to dying. When the virus is awake, and the cell is susceptible to dying, it kills itself but does not kill any other cells in the body.
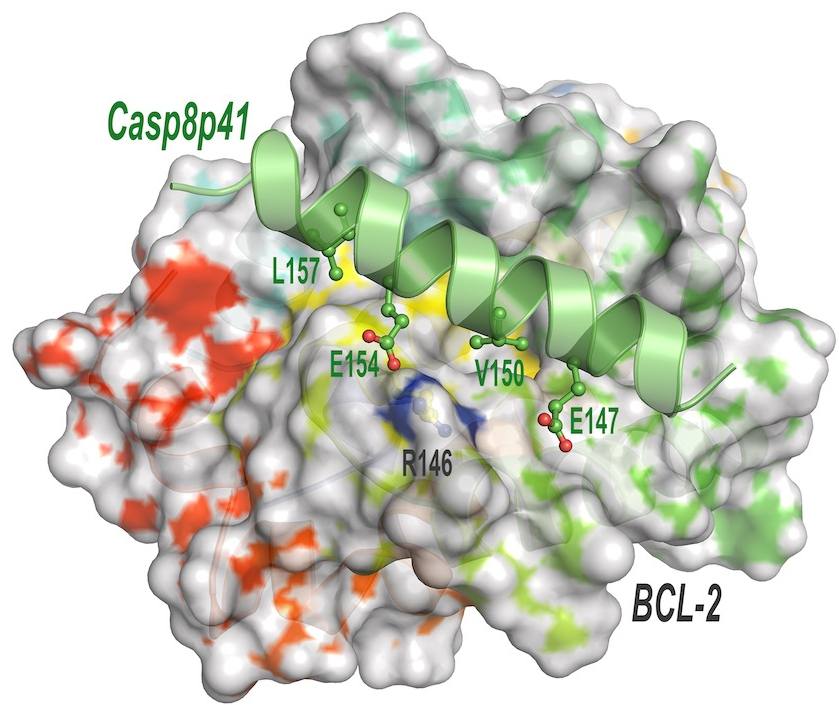
Essentially, it specifically targets the HIV-infected cells and eliminates them without hurting anything else. This new science is exciting. It's getting closer and closer to understanding how to do this effectively. And if you can do that with oral medications rather than fancy therapies like gene therapy or bone marrow transplant, it's scalable to large parts of the world, and you can touch millions of people that way. That's where the area of research is on how to make those hiding cells wake up, how to make them sensitive to die, and how to target just the HIV-infected cell.
Will we see a vaccine for HIV?
HIV has been a very hard vaccine to develop. In the world of viruses, vaccines fall into one of three buckets. They fall into the bucket where they respond to antibodies induced by the vaccine, and the vaccines are outstanding. Such viruses include polio, mumps, and lucky for us, SARS-CoV-2. Then we have the second category, like the influenza vaccine, which is about 60% effective. It certainly saves lives and makes a difference, but it's not perfect. And then we have the third bucket, which quite frankly is the vast majority of viruses that infect humans. And HIV is in that category, where simply forming an antibody to the virus is not adequate to prevent infection. You have to do very sophisticated engineering to induce T cell effects, as well as innate effects and antibody effects. Even then, sometimes it's very hard to decide what is the part of the virus to target. After decades, and billions of dollars of research, we're still not there for HIV. There have been many approaches of how to do this science. Many different scientific delivery mechanisms, many different areas of the viruses targeted, many different parts of the immune system targeted, and so far, none of them have been effective at preventing HIV infection.
What needs to happen next?
We still need to slow down the number of people getting infected through good public health measures and good education to stop the HIV epidemic. We still need to get more people who are infected on therapy.
We know we can do it with public health measures. But we also need to find out more about how we eliminate that reservoir and get people cured of the virus in a simple and effective way so that we can cure more people. And the last major hurdle we have is to develop an effective vaccine. We still don't have a vaccine that can prevent infection, a preventive vaccine, or a therapeutic vaccine where you give it to people who already have the virus that can help them control the infection. A huge amount of research has happened, but we're still not there yet.
Read more:
For the safety of its patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was recorded prior to COVID-19 or recorded in an area not designated for patient care, where social distancing and other safety protocols were followed.