-
What causes gastrointestinal bleeding and how serious is it really?

Gastrointestinal (GI) bleeding is a symptom of a disorder in your digestive tract. The blood often appears in stool or vomit but isn't always visible, though it may cause the stool to look black or tarry. The level of bleeding can range from mild to severe and can be life-threatening.
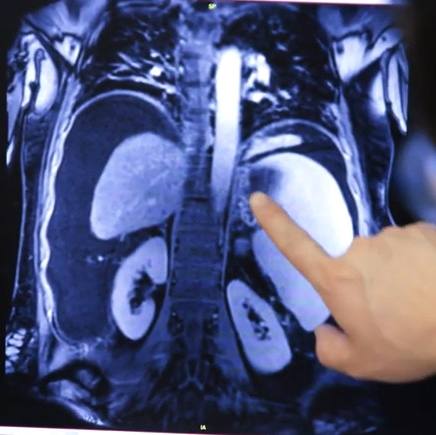
Sophisticated imaging technology, when needed, can usually locate the cause of the bleeding. Treatment depends on the source of the bleeding.
Symptoms
Signs and symptoms of GI bleeding can be either obvious (overt) or hidden (occult). Signs and symptoms depend on the location of the bleed, which can be anywhere on the GI tract, from where it starts — the mouth — to where it ends — the anus — and the rate of bleeding.
Overt bleeding might show up as:
- Vomiting blood, which might be red or might be dark brown and resemble coffee grounds in texture
- Black, tarry stool
- Rectal bleeding, usually in or with stool
With occult bleeding, you might have:
- Lightheadedness
- Difficulty breathing
- Fainting
- Chest pain
- Abdominal pain
Symptoms of shock
If your bleeding starts abruptly and progresses rapidly, you could go into shock. Signs and symptoms of shock include:
- Drop in blood pressure
- Not urinating or urinating infrequently, in small amounts
- Rapid pulse
- Unconsciousness
When to see a health care provider
If you have symptoms of shock, you or someone else should call 911 or your local emergency medical number. If you're vomiting blood, see blood in your stools or have black, tarry stools, seek immediate medical care. For other indications of GI bleeding, make an appointment with your health care provider.
Causes
Gastrointestinal bleeding can occur either in the upper or lower gastrointestinal tract. It can have a number of causes.
Upper GI bleeding
Causes can include:
- Peptic ulcer. This is the most common cause of upper GI bleeding. Peptic ulcers are sores that develop on the lining of the stomach and upper portion of the small intestine. Stomach acid, either from bacteria or use of anti-inflammatory drugs, damages the lining, leading to formation of sores.
- Tears in the lining of the tube that connects your throat to your stomach (esophagus). Known as Mallory-Weiss tears, they can cause a lot of bleeding. These are most common in people who drink alcohol to excess.
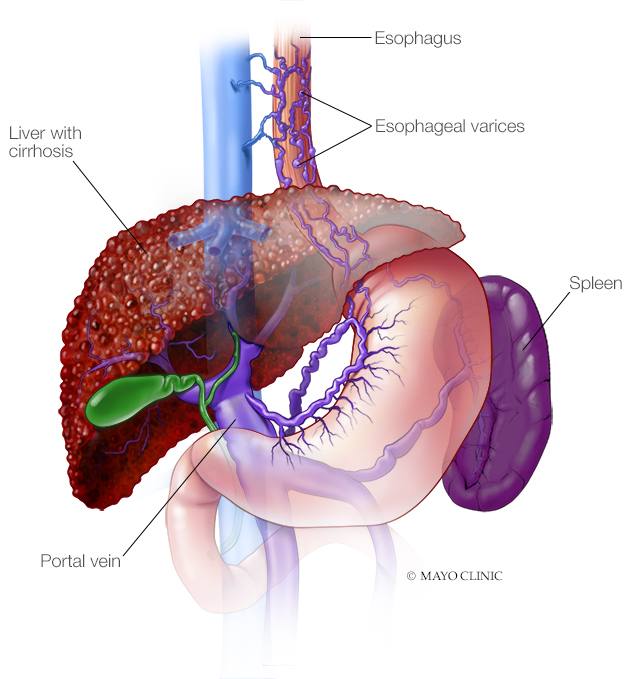
- Abnormal, enlarged veins in the esophagus (esophageal varices). This condition occurs most often in people with serious liver disease.
- Esophagitis. This inflammation of the esophagus is most commonly caused by gastroesophageal reflux disease (GERD).
Lower GI bleeding
Causes can include:
- Diverticular disease. This involves the development of small, bulging pouches in the digestive tract (diverticulosis). If one or more of the pouches become inflamed or infected, it's called diverticulitis.
- Inflammatory bowel disease (IBD). This includes ulcerative colitis, which causes inflammation and sores in the colon and rectum, and Crohn's disease, and inflammation of the lining of the digestive tract.
- Tumors. Noncanerous (benign) or cancerous tumors of the esophagus, stomach, colon or rectum can weaken the lining of the digestive tract and cause bleeding.
- Colon polyps. Small clumps of cells that form on the lining of your colon can cause bleeding. Most are harmless, but some might be cancerous or can become cancerous if not removed.
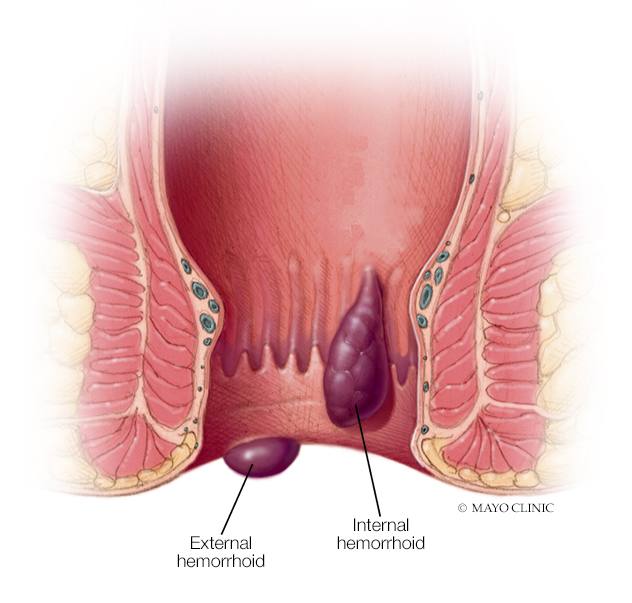
- Hemorrhoids. These are swollen veins in your anus or lower rectum, similar to varicose veins.
- Anal fissures. These are small tears in the lining of the anus.
- Proctitis. Inflammation of the lining of the rectum can cause rectal bleeding.
Complications
A gastrointestinal bleed can cause:
- Shock
- Anemia
- Death
Prevention
To help prevent a GI bleed:
- Limit your use of nonsteroidal anti-inflammatory drugs.
- Limit your use of alcohol.
- If you smoke, quit.
- If you have GERD, follow your health care provider's instructions for treating it.
____________________________________
This article is written by Mayo Clinic staff. Find more health and medical information on mayoclinic.org.