
The COVID-19 surge in cases continues across much of the U.S., and it is affecting every Mayo Clinic location across the Midwest. Testing volumes and positivity rates are increasing, and the number of patients who are hospitalized is rising, especially at Mayo Clinic in Rochester and Mayo Clinic Health System's Northwest Wisconsin Region.
Amy W. Williams, M.D., executive dean for practice, Mayo Clinic, is sharing plans that have been put in place at Mayo Clinic in Rochester and across Mayo Clinic Health System to respond to a spike in cases. She also answers these questions about the current situation with the surge and what the public needs to know to prevent them from becoming patients:
Watch: Dr. Amy Williams answers questions about the COVID-19 surge.
Journalists: Broadcast-quality sound bites with Dr. Williams are available in the downloads. Please courtesy: "Amy Williams, M.D. / Executive dean for practice / Mayo Clinic"
What is the current situation with the surge?
The situation is concerning. It's concerning for all of our communities that we have this many patients ― this many people ― that are ill with COVID-19 and need to be hospitalized.
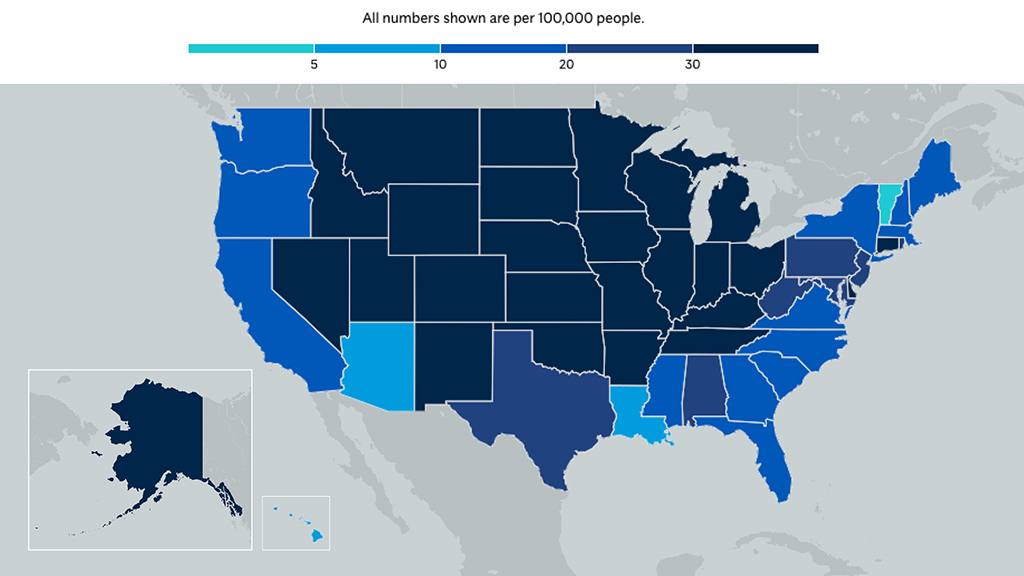
The numbers are increasing daily. And, in fact, for Mayo Clinic, what we have seen is an increasing number of tests that we are needing to supply to our communities ― because of symptoms ― is up to over 30,000 a week. To put that into perspective, last week, 30,671 tests were needed for our community. Prior to that, it was around 23,000. And throughout the summer, it was more like 13,000–14,000 a week. This just shows how our communities are seeing the spread of COVID-19.
How is this surge different than earlier this year?
We are in a very different place than we were in the spring. We know how to be safe. We are safe in our facilities. We also know how to treat COVID-19 patients. We have really robust modeling that allows us to prepare in advance for what we see coming down the road as far as COVID-19 surges and based on activities in our surrounding communities, and even further what's going on nationally. And we also model what we anticipate our staff exposures to be, and are looking at what staffing absences or gaps we may have.
What is the message that the public really needs to hear?
The most important things that our communities can do to decrease the spread and dampen the surge is to be safe. That means masking, social distancing and really robust hand hygiene. The other thing is to avoid risky situations where you can't socially distance and you can't mask. This is incredibly important to protect yourself and to protect others, and to get us back to where we want to be to open things up ― to open our world up. We can't do that until we all practice these safe measures.
What are the potential consequences to the system if we don't slow things down?
The most critical worry we have right now as far as our ability to care for patients is staffing. We have an increase in staff absences, and this may end up limiting our ability to care for patients. But we are mobilizing more staff into the inpatient setting, and to care for patients or individuals who have COVID-19 in the outpatient setting. With the community spread as high as it is, we need to make sure that we all stay incredibly safe.
What are Mayo's plans as we look at this surge, going into winter with the co-occurrence of COVID-19 and influenza?
First of all, masking and social distancing will help us with influenza also. And we've seen that in the countries in the Southern Hemisphere ― that those who were masking and social distancing because of COVID- 19, we have seen a significantly low incidence of people having influenza. We're hoping to see that same thing here. I do encourage everybody to get a flu vaccination. That's very important to help decrease influenza, as well as masking and social distancing. We are setting up testing. And in the near future, we will have testing ― simultaneous testing for COVID-19 and influenza ― based on symptoms.
Visitors
Hospital practice leaders at Mayo Clinic Hospital in Rochester implemented advanced visitor restrictions on Monday, Nov. 9, as part of the hospital's safety response to the ongoing COVID-19 pandemic. This means that Mayo will not allow visitors for patients at Mayo Clinic Hospital ― Rochester. Limited exceptions will be granted based on strict criteria specific to each patient's clinical situation. Mayo asks for the public's understanding in this matter.
At this time, Mayo has not changed its outpatient visitor policy.
Elective care
To address current and projected concerns amid increases in COVID-19 case volumes in the Midwest, the surgical practice is implementing contingency measures, including reductions of elective inpatient surgical cases. Each area of the surgical practice is evaluating its scheduled cases. Decisions to defer care will be made carefully and thoughtfully. Patients who are affected will be notified by Mayo Clinic.
Learn more about: Tracking and trending COVID-19
Information in this post was accurate at the time of its posting. Due to the fluid nature of the COVID-19 pandemic, scientific understanding, along with guidelines and recommendations, may have changed since the original publication date.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org.







