Make sure you have accurate information and understand related terminology to better understand COVID-19 and the spread of the virus. Below is a glossary of words that can help improve your COVID-19 knowledge during the pandemic.
This article is written by Mayo Clinic and Mayo Clinic Health System medical staff.
_________________________________
ACH
ACH refers to air changes per hour. In addition to wearing a mask and staying at least 6 feet away from other people, good air circulation indoors will reduce the spread of COVID-19. Increasing ventilation with outside air and using high-efficiency particulate air, or HEPA, filters and air purifiers can improve air quality. HEPA filters are effective in removing contaminants from the air and are common in most household appliances such as portable air purifiers, vacuum cleaners, heating, ventilation and air conditioning systems.
Antibody
An antibody is a blood protein produced in response to, and counteracting, a specific antigen. Antibodies help fight off infections and can protect against getting that disease again. That's called immunity. Antibodies are disease-specific. See definitions for "antigen" and "immunity" below.
Antibody test
COVID-19 antibody testing, also known as serology testing, is a blood test that's performed to find out if a person has had a past infection with SARS-CoV-2, the virus that causes COVID-19. An antibody test can't determine whether a person is currently infected with COVID-19.
Antigen
An antigen is a toxin or substance that the body recognizes as alien, such as bacteria or viruses in the blood, which induces an immune response in the body, especially the production of antibodies.
Antigen test
This COVID-19 test detects certain proteins in the virus. Using a long nasal swab or throat swab to get a fluid sample, antigen tests can produce results in minutes. Because these tests are faster and less expensive than polymerase chain reaction, or PCR, tests, antigen tests may be more practical to use for large numbers of people. Since there is an increased chance of false negative results, health care providers may recommend a polymerase chain reaction test to confirm a negative antigen test result. See the definition for "polymerase chain reaction test" below.
Asymptomatic test results
People who are asymptomatic have tested positive for a particular infection, such as COVID-19, but produce or show no symptoms. Although they may feel fine, they are infectious and can spread the virus to others.
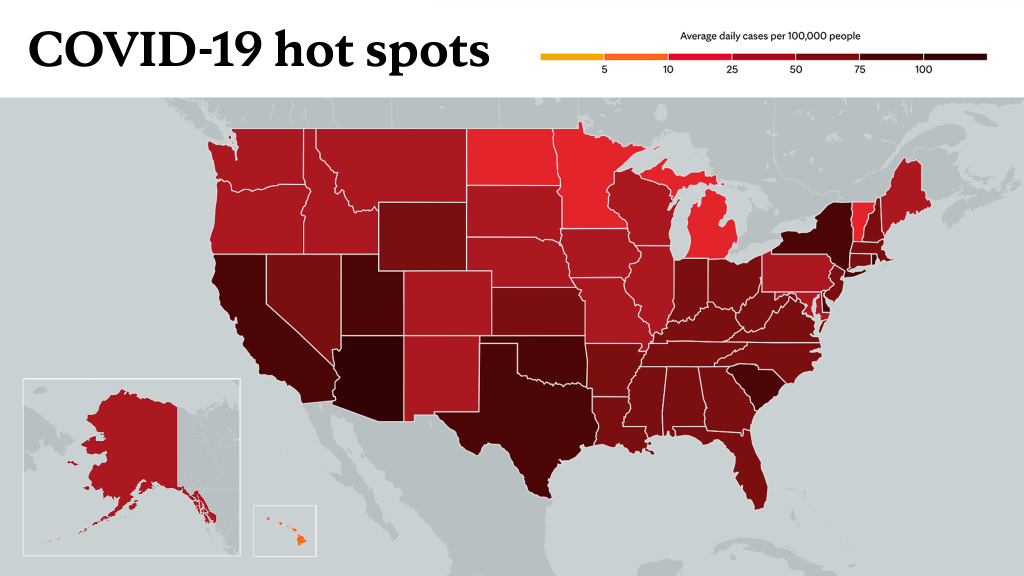
Community spread
The spread of an illness within a particular location, like in a neighborhood or town, is community spread. During community spread, there's no clear source of contact or infection. This is sometimes referred to as "community transmission." For the latest trends in COVID-19 cases near you, refer to Mayo Clinic's U.S. coronavirus map.
Contact tracing
Contact tracing helps protect people, family and community members, by:
- Letting people know they may have been exposed to COVID-19 and should monitor their health for signs and symptoms of COVID-19.
- Helping people who may have been exposed to COVID-19 get tested.
- Asking people to self-isolate if they have COVID-19 or self-quarantine if they are close contacts.
Coronavirus
Coronaviruses are a family of related viruses. Many coronaviruses cause respiratory illnesses. Coronaviruses cause COVID-19, severe acute respiratory syndrome, Middle East respiratory syndrome, and some strains of influenza or flu. The coronavirus that causes COVID-19 is SARS-CoV-2, which stands for "severe acute respiratory syndrome coronavirus 2."
COVID-19
COVID-19 is the name of the illness caused by SARS-CoV-2. COVID-19 stands for "coronavirus disease 2019."
COVID-19-negative
If people are COVID-19-negative, this means that they likely weren't infected with the COVID-19 virus. But a false negative test result could happen, depending on the timing and quality of the test sample. Even if they test negative, they could become infected in the future. Therefore, it's important to follow guidelines for social distancing, mask use and hand-washing to avoid potential spread. Their health care provider may recommend repeat testing if they continue to have symptoms.
COVID-19 outpatient therapy center
This outpatient service, which may be referred to as infusion therapy, administers remdesivir, which helps stop the virus from replicating and has been approved to treat the seriously ill, and bamlanivimab, a monoclonal antibody therapy, for use in high-risk patients who are experiencing less severe symptoms. Remdesivir needs to be administered intravenously daily for five days. Previously, patients who were otherwise ready for discharge might have remained in the hospital to complete their treatment. The COVID-19 outpatient therapy center allows them to finish it as outpatients. Bamlanivimab requires just one dose and has been shown to reduce the likelihood of disease progression.
As other medications become available, Mayo Clinic will be reviewing and adding treatments to care for patients.
COVID-19-positive
If people are COVID-19-positive, this means they have an active infection with the virus that causes COVID-19. They should take appropriate steps to care for themselves and avoid spreading the virus to others. They should self-isolate until they meet these three conditions:
- Their symptoms have improved.
- It's been three days since they've had a fever.
- It's been at least 10 days since their symptoms first appeared.
If they have severe symptoms of COVID-19 or a health condition that lowers their ability to fight disease, their health care provider may recommend that they stay in isolation longer. If they have a positive result but never developed symptoms, they should isolate for 10 days after the test.
Diversion
If a hospital runs low on beds, it can choose to temporarily divert patients elsewhere. However, a diversion does not mean the hospital will completely stop accepting new patients in an emergency. Diversion is often the last resort for hospitals. Diversion is only done when it is safe to send patients elsewhere and they are stable enough to make the journey.
Emergency department divert/bypass
The emergency department may go on a temporary divert/bypass when the volume or the acuity of the patients exceeds normal capabilities. Local emergency medical services, or EMS, is informed so they do not bring ambulances to the facility. However, patients who present through other means, such as car or walk-in, are triaged and treated as soon as possible.
Full hospital bypass
This is a temporary status for a health care facility in which all beds are full. The emergency room continues to triage and treat patients. If additional care is required and the patient is stable, the patient can be transferred to another organization.
Herd Immunity
Herd immunity occurs when a large portion of a community (the herd) becomes immune to a disease, making the spread of disease from person to person unlikely. As a result, the whole community becomes protected — not just those who are immune.
Often, a percentage of the population must be capable of getting a disease in order for it to spread. This is called a threshold proportion. If the proportion of the population that is immune to the disease is greater than this threshold, the spread of the disease will decline. This is known as the herd immunity threshold.
Immunity
Immunity is the body's ability to resist or fight off an infection. The immune system is a network of cells throughout the body that help a person avoid getting infected and help a person get better when infected.
Intensive care unit bypass
When the intensive care unit, or ICU, has reached capacity or based on the acuity of the patients and demands on staff, no other patients can be admitted.
Isolation or self-isolation
Isolation or self-isolation, also called self-quarantine, refers to separating sick people from healthy people to prevent spreading illness. Isolation keeps people who tested positive for COVID-19 with or without symptoms away from others, even in their own homes.
Monoclonal antibody treatment
Monoclonal antibodies are basically antibodies that will attach to the spike protein of the SARS-CoV-2 virus (the virus that causes COVID-19). What it does is once it attaches to that spike protein, the virus cannot attach itself to the cells, thereby limiting the spread of the infection and preventing it from progressing further.
Polymerase chain reaction test
This COVID-19 test detects genetic material of the virus using a lab technique called polymerase chain reaction, or PCR. A fluid sample is collected by inserting a long swab into a person's nostril and taking fluid from the back of the nose (nasopharyngeal swab) or inserting a long swab into the back of the throat (oropharyngeal swab), or spitting into a tube to get a saliva sample. Polymerase chain reaction tests are accurate when properly performed by a health care professional, but the rapid test can miss some cases.
Plasma donation
Researchers are testing the use of donated blood to treat people with severe COVID-19. People who find out that they are positive for the COVID-19 antibody may be eligible to donate plasma and help others. Learn more about plasma donation for COVID-19 from Mayo Clinic.
Personal protective equipment
Personal protective equipment, commonly referred to as "PPE," is equipment worn to minimize exposure to hazards that cause serious workplace injuries and illnesses. It may include gloves, isolation gowns, N95 masks, surgical face coverings, face shields or goggles.
Quarantine
Quarantining involves separating people who are asymptomatic and keeping them away from everyone else in the event that they might develop the disease. Quarantine also is appropriate for people who have been near people with known exposures.
Remote patient monitoring
Remote patient monitoring uses medical technology and devices that are sent to patients' homes so vital signs and symptom assessments can be screened every day. A team of nurses regularly monitors the data and contacts patients to assess health and progress toward health goals. The program was developed to support patients with complex chronic conditions, including those with COVID-19.
Superspreader
A superspreader is a person who is highly contagious and capable of transmitting an infectious disease to a large number of uninfected people.
Surge plan
In a disaster or pandemic situation when many patients require hospital admission, hospitals can activate what is called a surge plan. The surge plan brings together necessary resources like staffing and equipment to ensure the entire hospital works together to assign beds in the most efficient manner.
Virtual care
Through the benefits of technology, virtual care ― also referred as virtual visits, telemedicine, telehealth, video visits and phone visits ― allows people and their family to continue to receive the care they need while practicing social distancing during the COVID-19 pandemic. Virtual care options are available through Patient Online Services, the patient portal.
_____________________________________
Information in this post was accurate at the time of its posting. Due to the fluid nature of the COVID-19 pandemic, scientific understanding, along with guidelines and recommendations, may have changed since the original publication date.
For more information and all your COVID-19 coverage, go to the Mayo Clinic News Network and mayoclinic.org.
Learn more about: Tracking COVID-19 and COVID-19 trends