-
 Cancer
CancerLymph Node Ultrasounds More Accurate in Obese Breast Cancer Patients, Mayo Clinic Study Finds
 ROCHESTER, Minn. — Mayo Clinic research into whether ultrasounds to detect breast cancer in underarm lymph nodes are less effective in obese women has produced a surprising finding. Fat didn’t obscure the images — and ultrasounds showing no suspicious lymph nodes actually proved more accurate in overweight and obese patients than in women with a normal body mass index, the study found. The research is among several Mayo studies presented at the American Society of Breast Surgeons annual meeting April 30-May 4 in Las Vegas.
ROCHESTER, Minn. — Mayo Clinic research into whether ultrasounds to detect breast cancer in underarm lymph nodes are less effective in obese women has produced a surprising finding. Fat didn’t obscure the images — and ultrasounds showing no suspicious lymph nodes actually proved more accurate in overweight and obese patients than in women with a normal body mass index, the study found. The research is among several Mayo studies presented at the American Society of Breast Surgeons annual meeting April 30-May 4 in Las Vegas.
Researchers studied 1,331 breast cancer patients who received ultrasounds of their axillary lymph nodes, the lymph nodes in the armpits, to check for cancer before surgery. Of those patients, 36 percent were considered obese, with a body mass index of 30 or more. Body mass index is a formula that uses weight and height to estimate body fat. Of the other women studied, 33 percent were of normal weight and 31 percent were overweight but not obese.
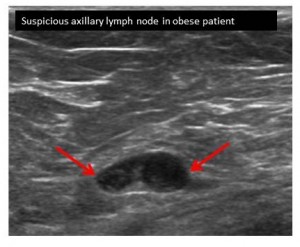
Obesity can change lymph nodes, including the way they look in imaging studies, and make physical examination of underarm lymph nodes more challenging. The Mayo study found that higher body weight didn’t muddy ultrasounds of the axillary lymph nodes in overweight or obese cancer patients, and that their ultrasounds had better specificity and accuracy than those of thinner women, meaning that when ultrasound showed no suspicious lymph nodes, it was likelier to be correct.
“I think we were surprised at these results,” says senior author Tina Hieken, M.D., a breast cancer surgeon at Mayo Clinic. ``It should be very reassuring that regardless of the weight of the patient, axillary ultrasound is helpful.”
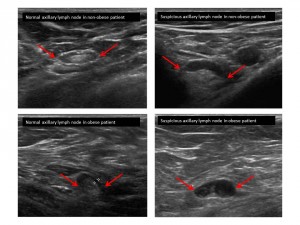 Potential reasons for the findings, Dr. Hieken speculates: Soft fatty tissue can be compressed during ultrasounds, and physicians now have more experience in knowing what lymph nodes may look like in overweight and obese patients. In some thin patients, ultrasounds may not yield as much information because underarm lymph nodes can be so close to the surface, it may be difficult to get good images, she says.
Potential reasons for the findings, Dr. Hieken speculates: Soft fatty tissue can be compressed during ultrasounds, and physicians now have more experience in knowing what lymph nodes may look like in overweight and obese patients. In some thin patients, ultrasounds may not yield as much information because underarm lymph nodes can be so close to the surface, it may be difficult to get good images, she says.
Surgeons do not rely on ultrasound alone to determine whether or not breast cancer has spread; it is one of several sources of information used to guide treatment.
“For most patients with invasive breast cancer, if the axillary ultrasound is negative, we perform a sentinel lymph node biopsy at the time of the breast operation to make sure cancer has not spread. When the preoperative axillary ultrasound shows suspicious lymph nodes, we then do a fine-needle aspiration of the lymph nodes. If that shows cancer, we may discuss other strategies with the patient such as giving chemotherapy before surgery,” Dr. Hieken says.
More research is planned, including looking at different techniques of lymph node ultrasound to improve accuracy and perhaps to avoid axillary lymph node surgery altogether in some breast cancer patients with small tumors and negative axillary ultrasounds, she says.
In other Mayo studies being presented at ASBS, researchers found:
- Using a regional anesthetic technique called a paravertebral block in breast cancer patients undergoing mastectomies reduces the need for narcotic painkillers after surgery and also means less postoperative nausea. The preoperative paravertebral block was used in addition to general anesthesia in 232 patients studied; they used fewer opioid painkillers and had less need for anti-nausea medication after surgery than 294 patients in the study who had mastectomies without the regional anesthetic.“From a patient standpoint, if they’re not nauseated and their pain is well-controlled, their entire surgical experience is better,” says senior author Judy Boughey, M.D., a Mayo Clinic breast surgeon.
- The rates of bilateral mastectomy, in which breast cancer patients have both breasts removed at once, were higher at hospitals where women could immediately have breast reconstruction surgery. At hospitals that offered immediate breast reconstruction, roughly 25 percent of women who had mastectomies had both breasts removed, compared to about 5 percent at hospitals that didn’t offer immediate breast reconstruction.“The advantage of the immediate breast reconstruction is ultimately fewer operations on the patient,” says Dr. Boughey, the senior author. Mayo Clinic offers immediate breast reconstruction after mastectomy; breast reconstruction begins and may even be completed in the same operation as the mastectomy.
###
About Mayo Clinic
Recognizing 150 years of serving humanity in 2014, Mayo Clinic is a nonprofit worldwide leader in medical care, research and education for people from all walks of life. For more information, visit 150years.mayoclinic.org, MayoClinic.org or https://newsnetwork.mayoclinic.org/.
MEDIA CONTACT: Sharon Theimer, Mayo Clinic Public Affairs, 507-284-5005, Email: newsbureau@mayo.edu







