-
Cancer
Creating Profile to Identify Patients Most at Risk of Developing Pancreatic Cancer
JACKSONVILLE, Fla. — When people find out — usually from a diagnostic scan looking at something else — that they have a lesion in their pancreas that could morph into pancreatic cancer, they can panic. They insist on having frequent CT scans and biopsies to monitor the lesion, or they ask for surgery. Physicians also don’t know if these abnormalities are dangerous, so the patients end up in surgery having part of their pancreas removed. Often the lesion is nothing to worry about.
But a team of international physicians, led by researchers at Mayo Clinic’s campus in Jacksonville, Florida, has developed a profile of the patient who would be most at risk of developing lesions that are most likely to develop into cancer. Their analysis is published online today in the journal Digestive and Liver Diseases.
“The factors we found that increase risk of pancreatic cancer now allow us to separate patients as either low or high risk,” says the study’s senior author, Michael B. Wallace, M.D., MPH, a gastroenterologist at Mayo Clinic. “High-risk patients can then be scanned and biopsied more frequently or can opt for surgery, but low-risk patients don’t need such surveillance. They can be watched much less intensively.”
MEDIA CONTACT: Kevin Punsky, Mayo Clinic Public Affairs, 904-953-0746, punsky.kevin@mayo.edu
“Pancreatic cancer is difficult to detect early — most patients are diagnosed at later stages when its 95 percent fatal — so we’re seeking ways to understand who is at risk,” Dr. Wallace says. “Our study offers valuable insight into the problem.”
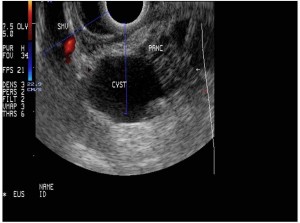
The lesions evaluated in this study that can become cancerous are known as intraductal papillary mucinous neoplasms. They are common. “Between 10 and 40 percent of people have them,” Dr. Wallace says. “Obviously the vast majority of those folks are not developing pancreatic cancer, which is not that common.”
To find ways to identify patients at high risk, Dr. Wallace and his collaborators, which include physicians at hospitals throughout the United States and Europe, examined data on 1,126 patients diagnosed with the lesions in the pancreas.
Of this group, only 84 were found to have invasive pancreatic cancer. Those patients had all or some of the following factors that put them at high risk: a history of smoking and obesity, and two symptoms of the disease—jaundice (yellowing of the eyes and skin) and steatorrhea (fat droplets in stool indicating that the pancreas was not producing sufficient digestive enzyme). Additionally, a larger cyst size on an imaging scan, cysts in the main pancreatic duct, and the presence of nodules on the cyst wall were all risk factors. Abdominal pain, which had been considered a risk factor, turned out not to be one in this study — patients at low-risk may have complained of such pain.
“This study refines the current guidelines for treating of these lesions, which are not very specific,” Dr. Wallace says. “Hopefully, we can assure worried patients who have these common lesions that they are not at high risk.”
Co-authors from Mayo Clinic include: Maria Moris, M.D.; Massimo Raimondo, M.D.; Timothy A. Woodward, M.D.; Verna Skinner. Co-authors from San Raffaele Scientific Institute, Milano, Italy include: Paolo G. Arcidiacono, M.D.; Maria C. Petrone, M.D. Claudio De Angelis, M.D. The co-author from Azienda Universitario-Ospedaliera San Giovanni Battista, Torino, Italy is Selene Manfre, M.D. The co-author from the University of Bologna/Hospital of Imola, Imola, Italy is Pietro Fusaroli, M.D.
###
About Mayo Clinic
Mayo Clinic is a nonprofit organization committed to medical research and education, and providing expert, whole-person care to everyone who needs healing. For more information, visit mayoclinic.com or newsnetwork.mayoclinic.org.
MEDIA CONTACT: Kevin Punsky, Mayo Clinic Public Affairs, 904-953-0746, punsky.kevin@mayo.edu







