-
Cardiovascular
Mayo Clinic Q and A: Family history and risk of peripheral artery disease
 DEAR MAYO CLINIC: I often get leg cramps and am wondering if I should get screened for peripheral artery disease, since my father had it. Are there other symptoms of peripheral artery disease I should be looking for?
DEAR MAYO CLINIC: I often get leg cramps and am wondering if I should get screened for peripheral artery disease, since my father had it. Are there other symptoms of peripheral artery disease I should be looking for?
ANSWER: Peripheral artery disease, or PAD, affects the arteries that supply oxygen and nutrients to the leg muscles. Leg cramping when you walk is one of its symptoms. The medical term for this is intermittent claudication. It usually goes away within a few minutes after you stop walking. A family history of peripheral artery disease can increase your risk for developing this disease, so it would be a good idea to see your health care provider and get tested for it.
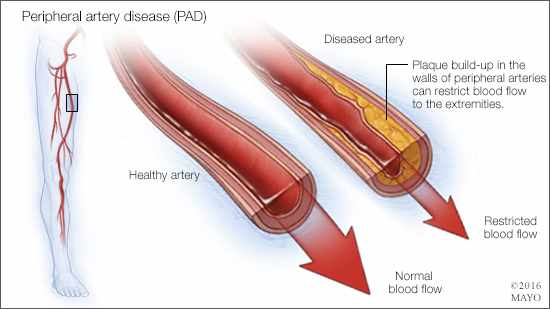
Peripheral artery disease happens when plaque builds up in your arteries, narrowing them and sometimes blocking them completely. When arteries are narrowed or blocked, the oxygen and nutrients in your blood can’t get to your tissues and muscles easily. The rate at which the plaque builds up and symptoms begin is different for every person.
Symptoms of peripheral artery disease often include tightness, cramping, weakness or numbness in the calf, thigh or buttocks when you walk. These symptoms can sometimes lead to leg weakness and falls. Other symptoms may include a cold feeling in your lower leg or foot; sores on your toes, feet or legs that won’t heal; a change in the color of your legs; hair loss or slower hair growth on your feet and legs; slow toenail growth; shiny skin on your legs; no pulse or a weak pulse in your legs or feet; and, in men, erectile dysfunction.
Your health care provider can diagnose peripheral artery disease using a test called the ankle-brachial index. It measures the blood pressure in your legs and compares it to the blood pressure in your arm. In people who don’t have peripheral artery disease, blood pressure in the legs is higher or equal to the one in the arm. People with peripheral artery disease have a much lower blood pressure in their legs.
People with PAD have a higher risk of heart attack or stroke. Effective treatment of peripheral artery disease often includes a combination of lifestyle changes and medication. In some cases, a procedure to open the arteries is necessary.
One of the best things you can do if you have peripheral artery disease is start walking on a regular basis. Walk for 30 minutes a day, at least four or five days a week. If that’s too much initially due to leg pain, then walk until, or just past, the maximum leg discomfort you can tolerate. Try to go a little farther every day, until you’re up to 30 minutes. The exercise will improve your heart and blood vessel health by improving oxygen delivery to your muscles, thereby helping your muscles work better and longer. Walking also promotes the growth of new blood vessels.
High cholesterol is a contributing factor to peripheral artery disease, and getting cholesterol under control is critical to successful peripheral artery disease treatment. Depending on your situation, you may need a statin medication to lower the level of cholesterol in your blood. Eating a healthy diet and maintaining a healthy weight can help lower cholesterol, too.
Other medical conditions that can worsen peripheral artery disease include uncontrolled diabetes and high blood pressure. If you have either of those conditions, talk to your health care provider about a treatment plan.
Finally, if you have peripheral artery disease and smoke, you need to stop. Smoking contributes to constriction and damage of your arteries and can make peripheral artery disease worse. If you smoke, quitting is the most important thing you can do to reduce your risk of peripheral artery disease complications. If you’re having trouble quitting on your own, ask your health care provider about smoking cessation options, including medications to help you quit. — Dr. Fadi Shamoun, Cardiovascular Diseases, Mayo Clinic, Scottsdale, Arizona







