-
Health & Wellness
Mayo Clinic Q and A: Absence of treatment, Crohn’s disease tends to get worse over time
DEAR MAYO CLINIC: My daughter is 19 and was recently diagnosed with Crohn’s disease. What is considered a flare-up? Her symptoms seem to be quite mild so far. Is it possible that this will continue, or do they usually worsen with time?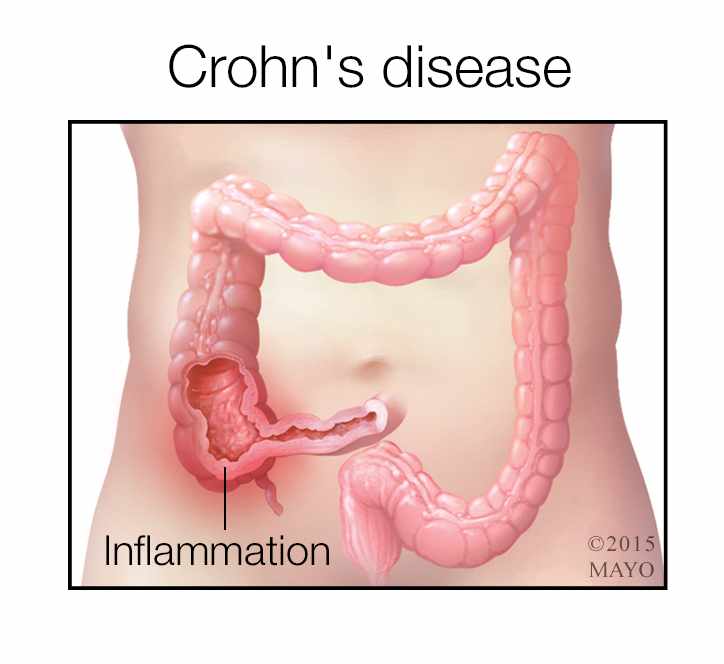
ANSWER: Crohn’s disease is a long-term condition that causes inflammation of the digestive tract lining. This inflammation can involve any part of the digestive tract, but it’s most common in the lower portion of the small intestine and in the large intestine. Unlike ulcerative colitis (another inflammatory condition), Crohn’s disease usually affects the entire thickness of the bowel wall.
People with Crohn’s disease typically have intermittent symptoms due to active inflammation. These are called flares. The flares usually alternate with periods of remission when there’s no active inflammation or symptoms. A flare may happen if a person with Crohn’s disease doesn’t take medication as prescribed, develops certain infections, receives antibiotics, or takes pain medications, including aspirin and nonsteroidal anti-inflammatory drugs such as ibuprofen and naproxen. Stress also may trigger a flare and result in symptoms of Crohn’s disease becoming worse.
The most common symptoms of a flare are abdominal pain and diarrhea. Other symptoms include rectal bleeding, nausea and vomiting, weight loss, fever, fatigue, pain and drainage around the anal area. People with Crohn’s disease may experience additional symptoms such as joint pains, painful red eyes or a skin rash. During a flare, symptoms can range from mild to severe, depending upon location of disease, length of the intestine involved and the degree of underlying inflammation. Those with early or mild disease usually have milder symptoms.
In the absence of treatment, Crohn’s disease usually tends to get worse over time and may result in serious complications. Complications can include narrowing of the intestine due to inflammation or scar tissue, called strictures; breakdown of tissue between the bowel and bladder, vagina, skin or other segments of bowel, a condition known as fistulae; and malnutrition. There’s also a risk of life-threatening complications, such as a bowel tear or perforation.
People diagnosed with Crohn’s disease in childhood or adolescence and those with perianal disease are at an increased risk of flares and disease progression. Smoking increases the risk of developing Crohn’s disease, leads to frequent flares and disease progression, and makes the need for surgery due to Crohn’s disease more likely.
Women with Crohn’s disease who would like to become pregnant should continue medical management for the disease and talk to their doctor. They should try to conceive when they are in remission, if possible. Women who conceive during a flare may continue to have symptoms throughout pregnancy. Stopping medications during pregnancy can also precipitate a flare and lead to pregnancy-related problems like miscarriage, premature delivery and low birth weight.
Without proper treatment, most people with Crohn’s disease eventually require surgery for disease-related complications. Surgery does not cure the disease, however, as Crohn’s often returns in the remaining part of the intestine. Although there is no cure, there are medications that can reduce inflammation, improve quality of life, avoid complications and prevent surgery. The goal of medical treatment is to prevent disease flares and maintain remission. The medications currently available are aminosalicylates, steroids, immunosuppressant agents and biologics.
Physicians use a combination of symptoms, lab tests, endoscopy and imaging exams to evaluate the disease and decide on the treatment that’s best for each individual. Medical therapy for Crohn’s disease often has to be taken for life. If flares continue, the physician may change medication dosages or recommend switching to a different medication. In addition to medical treatment, a healthy lifestyle, regular exercise, not smoking, yoga and meditation also may be beneficial in the management of Crohn’s disease. — Shabana Pasha, M.D., Gastroenterology and Hepatology, Mayo Clinic, Scottsdale, Ariz.
Related Articles







