 DEAR MAYO CLINIC: My mother was diagnosed with osteoporosis when she was in her 80s. My sister and I are now in our 60s, and my sister is concerned that we’re at high risk for the disease. I thought osteoporosis was just part of aging, especially for women. Can it run in families? Are there other things that can put a person at risk for it?
DEAR MAYO CLINIC: My mother was diagnosed with osteoporosis when she was in her 80s. My sister and I are now in our 60s, and my sister is concerned that we’re at high risk for the disease. I thought osteoporosis was just part of aging, especially for women. Can it run in families? Are there other things that can put a person at risk for it?
ANSWER: Although osteoporosis is more common as people age, it’s not a natural part of aging. There are a number of factors, including family history, that can raise your risk for osteoporosis.
Your body regularly makes new bone and breaks down old bone. When you’re young, your body makes new bone faster than it breaks down old bone, and your bone mass increases. Most people reach their peak bone mass in their mid-20s to mid-30s. The higher your peak bone mass, the more bone your body has to sustain bone health throughout the rest of your life.
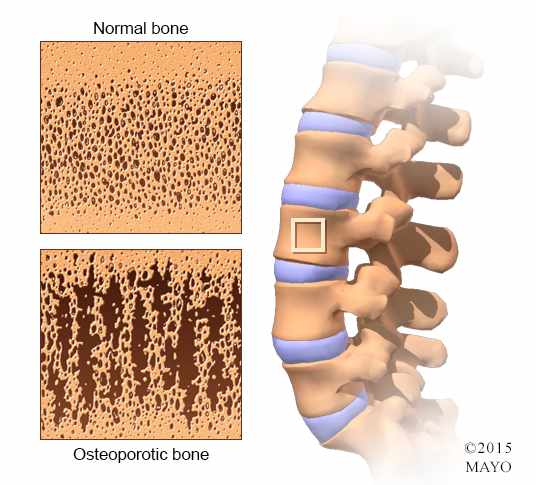
Osteoporosis risk rises with age because as you get older, you lose bone faster than your body can create it. Osteoporosis occurs when the body’s creation of new bone can no longer keep up with the breakdown of old bone. Bones then become weak, brittle and easily broken.
In addition to aging, research has shown that family history contributes to osteoporosis risk. If you have a parent or sibling with the disease, you are at greater risk, especially if your mother or father experienced a hip fracture.
Women are at higher risk, particularly those who are past menopause. That’s because women tend to lose bone density quickly in the years after menopause. That’s not to say men can’t get osteoporosis. About 20 percent of people diagnosed with the disease are male. Both men and women who have small body frames tend to have a higher risk because they may have less bone mass to draw from as they age.
Diabetes increases the risk. It’s been known for some time that type 1 diabetes contributes to the risk of osteoporosis. That’s because type 1 often starts in childhood and can have a negative impact on bone strength as people grow. More recently, though, it’s been found that people with type 2 diabetes also have an increased risk. It’s not clear why. This question currently is the subject of a considerable amount of research.
Diet can make a difference, too. A long-term lack of calcium plays a major role in the development of osteoporosis. Low calcium intake contributes to diminished bone density, early bone loss and an increased risk of fractures. Vitamin D deficiency can contribute to lower bone density over time, as well.
Another major risk factor for osteoporosis is a broken bone when you’re a child or young adult. Now, many children break bones. But they are often broken fingers and toes, or a broken arm or collarbone, that happen as part of a traumatic injury sustained during a vehicle accident or a sporting event. That’s not the type of broken bone that puts you at risk for osteoporosis.
Instead, if a bone breaks due to minor trauma when you wouldn’t expect it to in a child — as the result of a minor fall, for example — that could be a sign of predisposition to osteoporosis later in life. This is especially true if the broken bone is the wrist, hip, spine or shoulder.
If you’re concerned about your osteoporosis risk, talk with your doctor. In those who have never broken a bone and who don’t have other risk factors, it’s recommended that women have a bone density test to screen for osteoporosis at age 60. For men, it’s 70. If you’re younger than that and have risk factors, the test should be done sooner. For some people, depending on their level of risk, it could be as soon as age 50. — Bart Clarke, M.D., Endocrinology, Mayo Clinic, Rochester, Minn.
Related Articles







