-
Featured News
Mayo Clinic Q and A: Treating advanced emphysema with lung volume reduction
 DEAR MAYO CLINIC: How do doctors determine who is a good candidate for minimally invasive lung volume reduction to treat emphysema? Is it possible to have it done if I have only mild emphysema to slow the disease’s progression?
DEAR MAYO CLINIC: How do doctors determine who is a good candidate for minimally invasive lung volume reduction to treat emphysema? Is it possible to have it done if I have only mild emphysema to slow the disease’s progression?
ANSWER: The procedure you mention is intended for people who have advanced emphysema that no longer responds well to other treatments. It is not appropriate for cases of mild emphysema. The goal of minimally invasive lung volume reduction is to improve a patient’s quality of life by increasing breathing capacity.
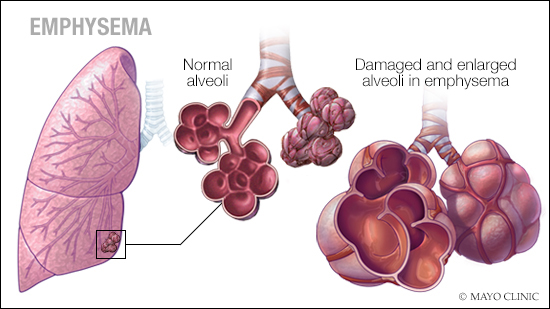
Emphysema is a lung disease in which the air sacs in the lungs, called “alveoli,” are damaged. In people who have emphysema, the inner walls of the air sacs weaken and rupture over time. That creates larger air spaces within the lungs, instead of many small ones, and leads to shortness of breath because less oxygen-rich air can get into the lungs. Other symptoms of emphysema include chronic coughing and difficulty breathing during exercise.
There’s no cure for emphysema, and it typically worsens over time. But treatment can ease symptoms and slow the rate of progression. That treatment usually includes medications, such as drugs to relieve coughing, shortness of breath and other breathing problems, as well as pulmonary rehabilitation that teaches techniques to improve breathing. In more severe cases of emphysema, supplemental oxygen may be necessary to relieve symptoms.
Lung volume reduction is a technique that can be used for people who have advanced emphysema and are receiving full treatment for it but still have shortness of breath that limits their ability to perform daily activities.
Traditional lung volume reduction involves surgery to remove small wedges of damaged lung tissue. Removing that tissue allows the remaining lung tissue to function better, thereby improving breathing.
More recently, a minimally invasive technique that does not require open surgery has been developed to reduce lung volume. During that procedure, which takes about an hour, the patient is given general anesthesia. A physician puts a small endoscope through the mouth, down into the lungs, and positions it within the areas of the lungs identified as being the most damaged. Using a small catheter within the endoscope, tiny one-way valves are then placed in the damaged areas. The valves allow air to get out, but no fresh air can get in. The result is that the sections of the lungs most affected by emphysema deflate and shrink over time. That allows the rest of the lung tissue to have more space to expand and function, so the patient can take a deeper breath and get more oxygen into the bloodstream.
One of the main benefits of the minimally invasive approach to lung volume reduction is that it doesn’t involve traditional surgery. That means people who may not otherwise be good candidates for lung volume reduction due to health concerns that could make surgery unsafe, such as those who are obese or have cardiovascular disease, may be able to have the procedure done with this new technique. In addition, the minimally invasive procedure typically results in less scarring and pain afterward, and it usually requires a shorter hospital stay than surgery.
After lung volume reduction, many people can reduce or eliminate their dependence on supplemental oxygen. It often significantly affects how well these individuals can perform their daily activities, too. Tasks such as walking up a flight of stairs, shopping at the grocery store and exercising become easier.
Although lung volume reduction won’t cure emphysema, and treatment with medication still may be necessary after the procedure, lung volume reduction often can significantly improve exercise capacity, lung function and quality of life for people with severe emphysema. — Dr. Sebastian Fernandez-Bussy, Pulmonary and Critical Care Medicine, Mayo Clinic, Jacksonville, Florida
****************************
Related Article
- Mayo Clinic Q and A: Rare, inherited risk factor can result in emphysema and liver damage published 1/15/19







