-
Multiple myeloma: Its evolution, treatment and the quest to catch it early

Multiple myeloma is a cancer of a type of white blood cell called a plasma cell in the bone marrow. When multiple myeloma develops in the bone marrow, cancerous plasma cells multiply, crowding out healthy cells.
"Over time, people develop abnormalities or mutations in their plasma cells. Those mutations cause plasma cells to become cancerous," says Joselle Cook, M.B.B.S., a Mayo Clinic hematologist specializing in multiple myeloma and other plasma cell disorders. "Older age is a risk factor. Multiple myeloma is commonly diagnosed in people in their 60s and 70s. We also know that Black people develop myeloma about 10 years earlier than white people, and two to three times more frequently."
Having a family history of multiple myeloma may also increase the risk of the disease.
An estimated 35,780 new cases of multiple myeloma will be diagnosed in the United States in 2024. While multiple myeloma is a serious condition, people with the disease are living longer because treatments have advanced. "The prognosis has changed remarkably over the last few years," says Dr. Cook.
Read on for an overview of how multiple myeloma evolves, how healthcare professionals treat it, and the quest to find a screening test to diagnose the disease before it can damage the body.
The evolution of multiple myeloma
Cancerous plasma cells — myeloma cells — make proteins that cause the symptoms and complications of multiple myeloma. "When the plasma cells develop mutations and produce a monoclonal protein, this group of conditions is called monoclonal gammopathies," says Dr. Cook.
The earliest phase of monoclonal gammopathies is monoclonal gammopathy of undetermined significance (MGUS), which doesn't cause symptoms. When a person has MGUS, monoclonal protein, or M-protein, is found in their blood at a level too low to damage the body. "If we detect M-protein in a person's blood, and we aren't concerned about organ damage, we monitor them," says Dr. Cook.
If cancerous plasma cells continue to multiply and produce M-proteins, MGUS evolves into smoldering multiple myeloma. People still don't have symptoms at this phase but have a higher M-protein level in their blood and urine.
People with smoldering multiple myeloma are classified based on their risk of progressing to multiple myeloma: low risk, intermediate risk or high risk. "We may treat some people with high-risk smoldering multiple myeloma, typically as part of a clinical trial, but for the most part, we actively monitor people without treating them," says Dr. Cook.
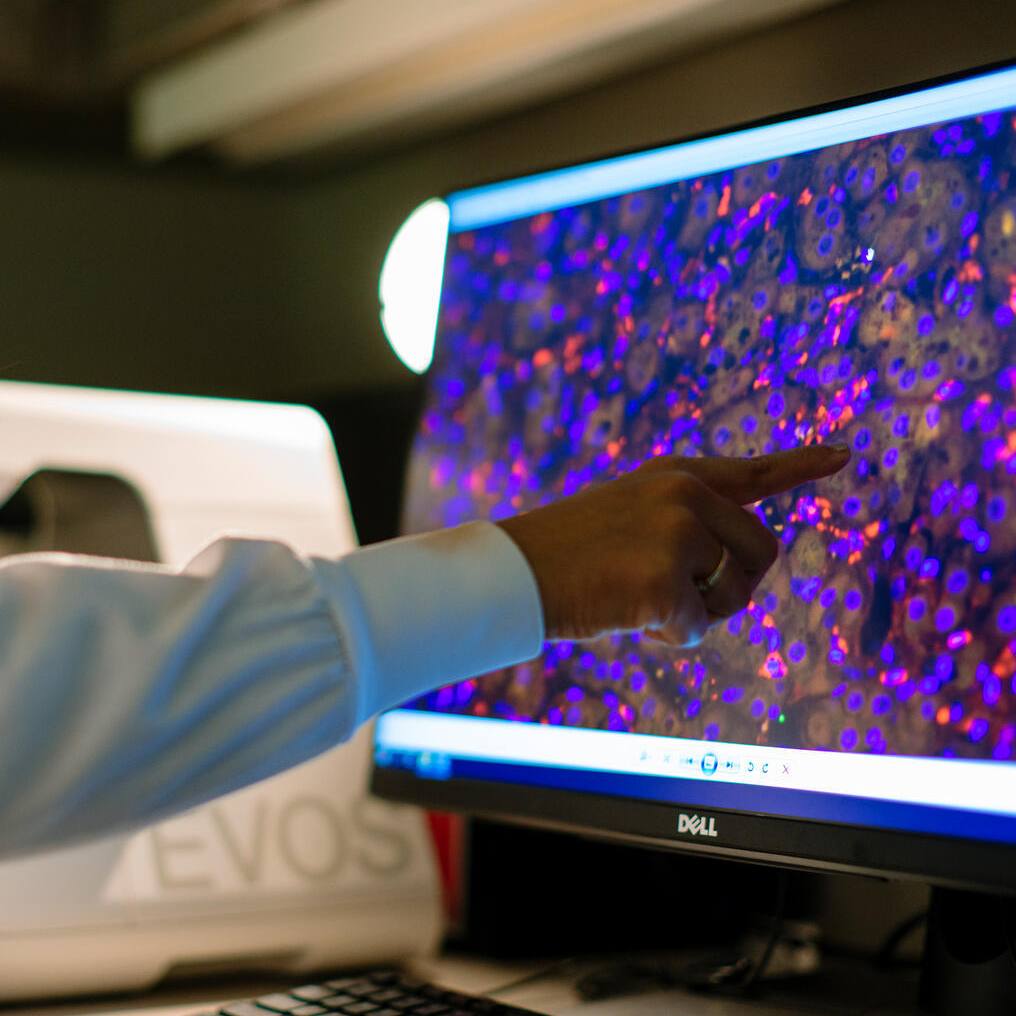
Multiple myeloma might be suspected when blood tests conducted for another reason raise red flags. "We may see that the protein is quite elevated or that a patient has a lower blood count than usual or an abnormality in their kidney numbers," she says. This prompts a care team to order blood tests to detect M-protein and assess blood chemistry and kidney function, urine tests to detect proteins, imaging tests to identify bone problems, and a bone marrow biopsy to look for myeloma cells.
People with multiple myeloma can experience a variety of symptoms or none. This can make diagnosing the disease a challenge. When a healthcare professional suspects multiple myeloma, they frequently check for specific signs and symptoms. "People with multiple myeloma may have anemia. If the M-proteins deposit in the kidneys and cause them to fail, they will have kidney abnormalities. They may have bone pain and high blood calcium levels caused by bone destruction," says Dr. Cook.
Multiple myeloma treatment options
Treatment for multiple myeloma typically starts with a combination of medications called induction chemotherapy. "Treatment involves plasma-cell directed therapy," says Dr. Cook. "It's usually a combination of three or four drugs: A steroid, an immunomodulating agent (a drug that stimulates the immune system to fight cancer), an antibody (anti-CD38) that targets a surface marker on the cancerous plasma cell, and a proteasome inhibitor that targets the cell's protein manufacturing."
Your care team will also decide if you are a candidate for a bone marrow transplant. "This decision depends on factors like fitness and age — it's a soft cut-off, but generally, we don't transplant patients over 75. There are exceptions, though," says Dr. Cook.
The drugs your care team uses in your induction chemotherapy will depend on your overall health and whether you are a candidate for a bone marrow transplant.
A bone marrow transplant — a stem cell transplant — is a procedure that infuses healthy blood-forming stem cells into your body to regenerate the bone marrow's ability to produce blood cells. Stem cell transplants can pose risks, and some people can have serious complications.
If eligible, people with multiple myeloma typically have a stem cell transplant after about four to six months of induction chemotherapy. Before the transplant, they receive a high dose of a different type of chemotherapy called conditioning chemotherapy.
Dr. Cook uses a garden metaphor to explain how conditioning and stem cell transplants work to treat multiple myeloma. "In myeloma, your bone marrow is akin to a garden overgrown with weeds (the myeloma). You use strong weed killers (the conditioning chemotherapy) to eliminate those weeds, but then the garden is barren. You need to plant seeds to allow the garden to grow. That's what a stem cell transplant does. The reinfusion of stem cells is like planting seeds so your bone marrow can recover faster."
Dr. Cook says other promising treatment options exist if you cannot undergo a bone marrow transplant. "For people who relapse after several types of treatment, CAR-T cell therapy, where people's T cells are engineered to recognize and kill a myeloma cell, offers great response rates and good survival. And we've seen success with new drugs called bispecific antibodies — specially designed antibodies that redirect a patient's T cells (immune cells) to kill myeloma cells," she says.
Radiation therapy may also be an option to treat areas of the body affected by myeloma that are painful or causing other problems, says Dr. Cook.
Research aimed at catching multiple myeloma early
"Being diagnosed early is important because you want to avoid organ damage, renal impairment and bone destruction. If we can detect and diagnose multiple myeloma early, we can prevent that damage," says Dr. Cook.
"MGUS and multiple myeloma are detected most often. It's less common to detect smoldering multiple myeloma," says Dr. Cook. She says researchers are exploring screening options — primarily blood tests — to identify MGUS and smoldering myeloma.
Dr. Cook is working with colleagues on a clinical trial in Rochester, Minnesota, to screen people of East African descent. Other clinical trials are studying people with MGUS and those in higher-risk populations. "There are screening studies focused on Black people and those who have first-degree relatives with myeloma or MGUS," she says.
Dr. Cook is confident that the outlook for people diagnosed with multiple myeloma will continue to improve. "There are so many treatment options being developed," she says. "The field is just forging ahead."
Learn more
Learn more about multiple myeloma and find a clinical trial at Mayo Clinic.
Join the Blood Cancers and Disorders Support Group on Mayo Clinic Connect, an online community moderated by Mayo Clinic for patients and caregivers.
This article first published on the Mayo Clinic Comprehensive Cancer Center Blog.