-
Research
New discovery may unlock regenerative therapies for lung disease
When a person's lungs are damaged, that organ's survival depends on a small but powerful set of cells that must choose whether to repair the tissue or fight infection. A new Mayo Clinic study has uncovered the molecular "switch" that directs these cells down one path or the other, a discovery that could inform regenerative therapies for chronic lung diseases.

"We were surprised to find that these specialized cells cannot do both jobs at once," says Douglas Brownfield, Ph.D., senior author of the study, which was published in Nature Communications. "Some commit to rebuilding, while others focus on defense. That division of labor is essential — and by uncovering the switch that controls it, we can start thinking about how to restore balance when it breaks down in disease."
It takes two
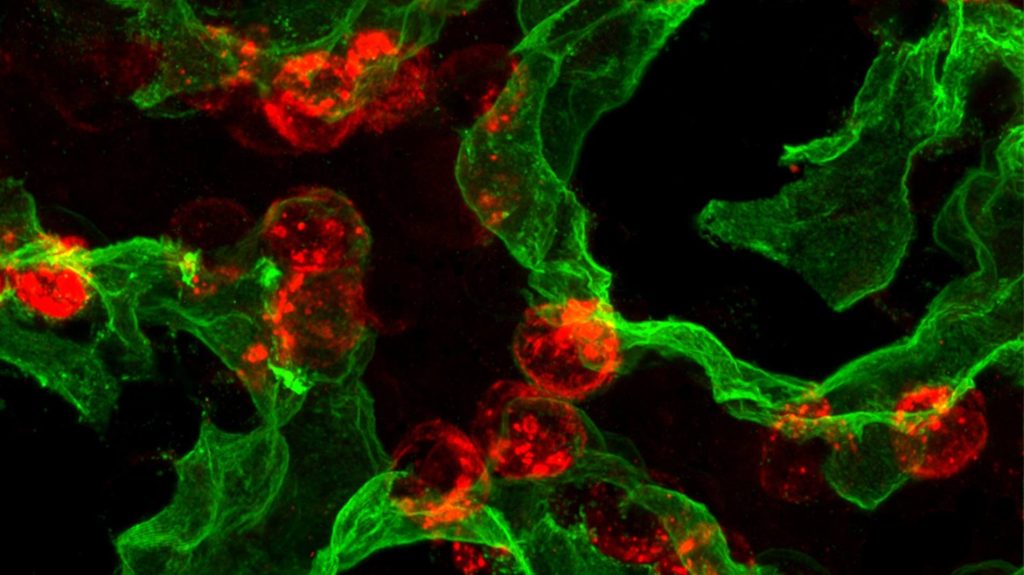
The new research centers on alveolar type 2 (AT2) cells, which play a dual role in the lung. These cube-shaped cells secrete surfactant proteins that keep air sacs open, but they also act as reserve stem cells capable of regenerating alveolar type 1 (AT1) cells — the paper-thin cells that form the surface for gas exchange. This regenerative capacity makes AT2 cells essential for lung repair after injury.
For decades, scientists have known that these cells often fail to regenerate properly in lung diseases such as pulmonary fibrosis, chronic obstructive pulmonary disease (COPD) and severe viral infections like COVID-19. What remained unclear was how AT2 cells lose their stem cell capacity.
Using single-cell sequencing, imaging and preclinical injury models, the team mapped the developmental "life history" of AT2 cells. They found that newly formed AT2 cells stay flexible for about one to two weeks after birth before "locking in" to their specialized identity.
That timing is controlled by a molecular circuit involving three key regulators called PRC2, C/EBPα, and DLK1. The researchers showed that one of them, C/EBPα, acts like a clamp that suppresses stem cell activity. In adult lungs, AT2 cells must release this clamp after injury to regenerate.
The same molecular switch also directs whether AT2 cells repair lung tissue or defend against infection. That helps explain why infections often slow recovery from lung disease.
"When we think about lung repair, it's not just about turning things on — it's about removing the clamps that normally keep these cells from acting like stem cells," says Dr. Brownfield. "We discovered one of those clamps and how it times the ability of these cells to repair."
Preventing organ failure
The discoveries could guide the development of therapies to fix AT2 cells that are broken in disease. Drugs that target C/EBPα, for example, may restore repair programs or reduce scarring in pulmonary fibrosis.
"This research brings us closer to being able to boost the lung's natural repair mechanisms, offering hope for preventing or reversing conditions where currently we can only slow progression," says Dr. Brownfield.
The findings may also guide earlier detection, helping clinicians identify when AT2 cells are stuck in one state and unable to regenerate. Such insights could lead to new biomarkers for lung disease. This work aligns with Mayo Clinic's Precure initiative, which focuses on detecting disease at its earliest stages — when interventions are most effective — and preventing progression before organ failure occurs.
At the same time, the research advances Mayo Clinic's Genesis initiative, which aims to prevent organ failure and restore function through regenerative medicine. The team is now testing strategies to remove the repressive clamp on human AT2 cells, expand them in culture and potentially use them for cell replacement therapy.







