-
Science Saturday: Researchers find widespread sex bias in molecular biology tools
Widely used sex-biased maps of molecular biology are holding back individualized medicine, say Mayo Clinic scientists.
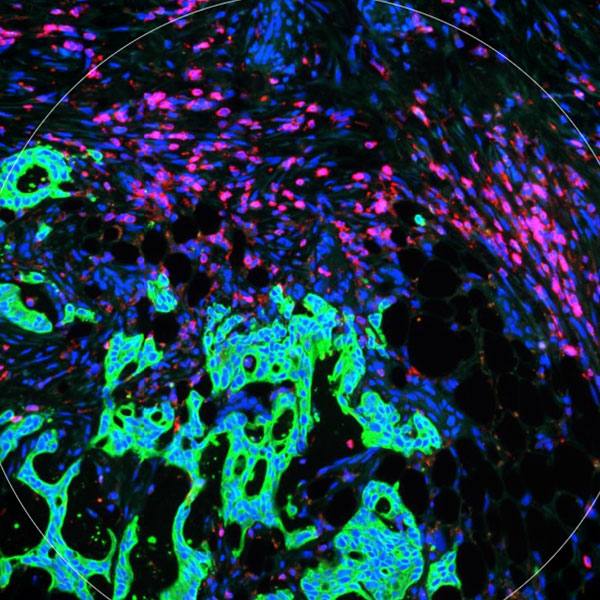
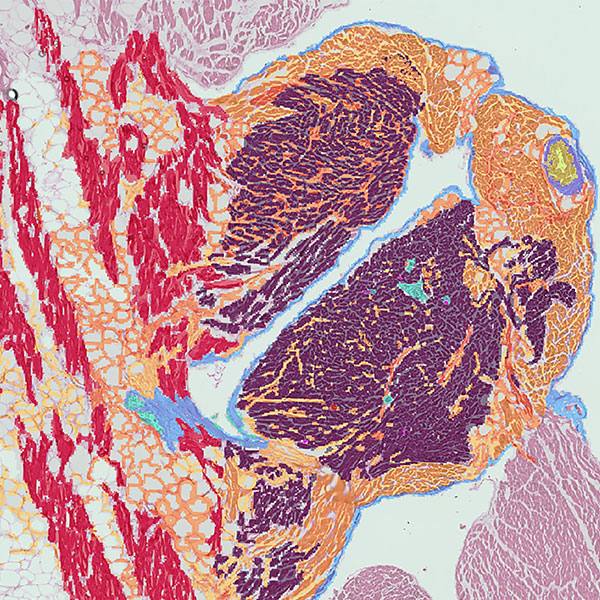
Maps clarify how places are connected. In biology, the same is true for databases that map out how aspects of biology are connected. Different biological databases examine genes (genomics), how those gene instructions are read (transcriptomics), what is made from the gene instructions (proteomics), and how that gene product breaks down in the body (metabolomics). Called omics for simplicity, these mapping tools are routinely used in biomedical research to understand what is happening on a molecular and cellular level in normal and disease states.
While extremely useful for researchers, a Mayo Clinic-led commentary published in Nature Methods found that relying on omics tools can introduce bias related to sex differences that could contribute to misleading results.
"These tools leverage databases that summarize all known molecular interactions, the vast majority of which were discovered using male-biased study designs," says Kamila Bond, first author of the study. She is a member of the Mathematical Neuro-Oncology lab at Mayo Clinic in Arizona, led by Kristin Swanson, Ph.D., a mathematical oncologist.
While these tools are extremely popular, Bond says, the default male standard fails to account for the fundamental sex differences between males and females in biology.
"These databases are used as maps," adds Dr. Swanson, "for interpreting essentially every biological analysis across all of biomedicine. This limits our ability to even identify, let alone study, potential sex differences that can and do exist across a spectrum of diseases. Unless we act, our hopes for making individualized medicine truly individualized are stuck ignoring entire chromosomes of our biology. Further, these biased tools also hamper our ability to distinguish differences in gender as distinct from sex, race, age and other elements of diversity."

The article reported the following observations:
- If the database is male-biased, but there are truly no sex differences in the system, the output will be accurate for both males and females
- If sex differences exist within certain medical conditions and the database is male-biased, the results could be:
- accurate for males but have lower significance in females
- incomplete in females
- uninformative in females
- If sex differences exist and the database is female-biased, results may be uninformative for males
- If the database annotates for sex, allowing for truly sex-specific analyses, male and female outputs can be both different and accurate
"If we truly want to advance patient care for both males and females, we must acknowledge the intrinsic historical male bias of research, retrospectively try to correct for this bias, and ensure that appropriate diversity is incorporated into study designs," says Bond.
She adds that a more diverse database could identify key individual differences in patients that could lead to a more individualized approach in treating patients across a spectrum of diseases.
Alice Chang, M.D., director of Mayo Clinic's Transgender and Intersex Specialty Care Clinic, adds another aspect that could affect metabolomics: the intersection of sex hormonal changes with puberty, conditions of hormone deficiency or excess, and transgender people.
"It is not known how known sex differences in cisgender phenotypes might change with gender-affirming hormone therapy or surgeries that include gonadectomy," says Dr. Chang. "Once natal sex differences are identified in metabolomics, follow-up validation studies could examine the influence of sex steroid hormones on identified sex differences."
Dr. Swanson, Bond, and co-authors provide detailed recommendations in the paper for biomedical scientists, database curators, and funding agencies to consider to improve the current system. A complete list of authors and funding information can be found within Nature Methods.