-
Health & Wellness
TUESDAY Q & A: Surgery can usually treat urinary incontinence, but less invasive options are available
DEAR MAYO CLINIC: I am 43 and have had trouble with urinary incontinence since having my fourth child at 41. It seemed manageable until about 6 months ago when I started to notice it happening more frequently. At what point should I consider surgery?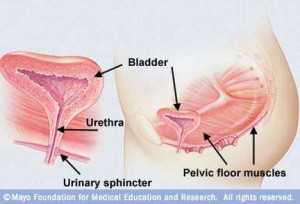
ANSWER: Urinary incontinence is a common problem for women, especially after pregnancy and childbirth. Surgery usually can effectively eliminate urinary incontinence. But less invasive treatment options are available that you can try before turning to surgery.
Urinary incontinence, or loss of bladder control, affects about half of all women at some point during their lifetimes. Factors that increase the risk of urinary incontinence include age, childbirth and pelvic floor muscle weakness.
Although there are several different types of urinary incontinence, the kind that women in your situation most often have is stress incontinence. With stress incontinence, urine leaks when pressure or stress is placed on the bladder, such as when you cough or sneeze, when you lift something heavy, or when you exercise.
During a medical evaluation of urinary incontinence, your doctor will talk with you about your medical history and your symptoms. The appointment will likely include a physical exam that involves checking the strength and tone of your pelvic floor muscles, as well as assessing the support of your pelvic organs, particularly those of the bladder and urethra.
A urinalysis usually is part of the initial assessment, too. This lab test analyzes a sample of your urine to check for a medical condition that could be causing urinary incontinence. A urinary tract infection, for example, can often trigger loss of bladder control. If an underlying problem is detected, treating that condition may eliminate urinary incontinence.
To further assess your situation, your doctor may ask you to keep a diary for several days that tracks your bladder habits and symptoms. In this log, you record how often you urinate, the number of leaks you have, and the amount and types of fluid you drink. Based on that, your doctor may recommend you try timed voids or change the type or amount of fluid you drink.
If your evaluation shows that stress incontinence is the problem, the first step in therapy may include exercises to help strengthen your pelvic floor muscles. Also, if your pelvic floor muscles are weak, a device called a pessary may be useful. It is placed in the vagina to support the bladder and bladder neck.
Injectable bulking agents can be used to treat stress incontinence, too. Bulking agents are materials injected into tissue surrounding the urethra. They help keep the urethra closed and reduce urine leaks. The injection is usually done in a doctor’s office and takes only a few minutes. This procedure may be helpful for women who cannot have or do not want surgery, but who have tried other medical treatment without success.
If symptoms persist after conservative therapy, then the next step would be to consider surgical treatment. Surgery offers high cure rates for urinary incontinence, but it is invasive. Several surgical approaches are available.
For example, a sling procedure uses strips of your body’s tissue, synthetic material or mesh to create a pelvic sling or hammock around your bladder neck and urethra. The sling helps keep the urethra closed, especially when you cough or sneeze. Another option is a bladder neck suspension. This surgery provides added support to the urethra and bladder neck — the area where the bladder connects to the urethra. The process of deciding on a surgical procedure depends on several factors, including whether or not there is associated pelvic organ prolapse that needs to be corrected.
Before you consider surgery, make an appointment to see your doctor to have your condition thoroughly evaluated. Based on that evaluation, you can make a treatment plan that fits your needs. — Anita Chen, M.D., Gynecologic Surgery, Female Pelvic Medicine and Reconstructive Pelvic Surgery, Mayo Clinic, Jacksonville, Fla.
Related Articles







