DEAR MAYO CLINIC: Is preventative surgery an option for people with a strong genetic predisposition to pancreatic cancer? If not, are there any screening tests that can catch it early?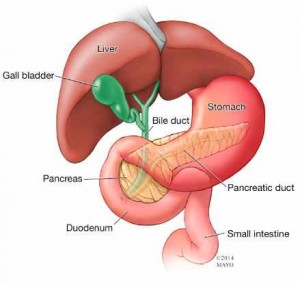
ANSWER: Although removing the pancreas is a possibility for people who have a strong family history of pancreatic cancer, it is used only rarely as a means of preventing the disease. That’s because there are significant health risks associated with not having a pancreas. No formal screening methods are in place for this type of cancer. But certain imaging exams may be able to detect pancreatic cancer in its early stages.
Your pancreas is located in your abdomen, behind the lower part of your stomach. One of its main jobs is to make insulin, a hormone that regulates the transfer of sugar, or glucose, from your bloodstream into your cells. The pancreas also makes enzymes that aid in your body’s digestion.
Pancreatic cancer starts in the tissue of the pancreas. In its early stages, it seldom causes signs or symptoms. This cancer often spreads quickly and is difficult to successfully treat. In general, pancreatic cancer is not common. If you have a family history of the disease, though, your risk of developing pancreatic cancer can be two to three times higher than normal.
Given the increased risk and the poor outlook for those diagnosed with pancreatic cancer, it is reasonable for people who have multiple relatives with the disease to seriously consider their options for reducing the risk of pancreatic cancer or for catching it in its early stages.
Removing the pancreas may seem like a straightforward way to prevent cancer. But that procedure is associated with a number of serious long-term side effects. People who do not have a pancreas often develop diabetes that is hard to control. That, in turn, can bring with it a host of other significant medical issues. In addition, if you do not have a pancreas, you are at an increased risk of developing heart disease.
That said, for people who have a significant family history of pancreatic cancer, it may still be worthwhile to consider pancreas removal. A medical team usually will only move forward with this surgery, however, after thorough discussion and consultation with all the medical specialty areas involved to review the individual benefits and risks.
There are ways to monitor a person who is at high risk for pancreatic cancer. Although the specific tests used and how often they are recommended depend on your health and family history, several imaging exams can screen for pancreatic cancer, including CT scans and MRI studies. The test that is often the most useful, though, is an endoscopic ultrasound.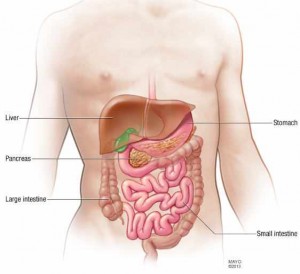
An endoscopic ultrasound uses an ultrasound device to create images of your pancreas from inside your abdomen. The device is passed through a thin, flexible tube, called an endoscope, down your esophagus and into your stomach to obtain the images.
In some cases, the results from these imaging tests can be difficult to read because people at high risk for pancreatic cancer tend to have existing abnormalities in the pancreas, which can sometimes make it hard to accurately identify cancerous tumors.
You may be able to lower your risk of pancreatic cancer by not smoking, staying at a healthy weight and eating a diet that includes plenty of vegetables, fruits and whole-grain foods. Be aware of the symptoms of pancreatic cancer, too. Common symptoms include deep aching back pain, weight loss, nausea, vomiting, yellowing of the skin and light-colored stools. If you notice any of these, report them to your doctor right away.
If you have a family history of pancreatic cancer, talk to your doctor about your risk of the disease and steps you can take to lower that risk. Also, ask about creating a schedule for ongoing monitoring and follow-up care. — KMarie Reid Lombardo, M.D., M.S., Surgery, Mayo Clinic, Rochester, Minn.







