-
Women’s Wellness: Eating fish during pregnancy

If you're unsure about whether it's safe to eat seafood during your pregnancy, you're not alone. Pregnancy nutrition can be confusing, especially when it comes to seafood guidelines. Here's help understanding the facts.
What are the pros and cons of eating seafood during pregnancy?
Seafood, which includes fish and shellfish, can be a great source of protein, iron and zinc — crucial nutrients for your baby's growth and development. The omega-3 fatty acids in many fish, including docosahexaenoic acid (DHA), also can promote your baby's brain development.
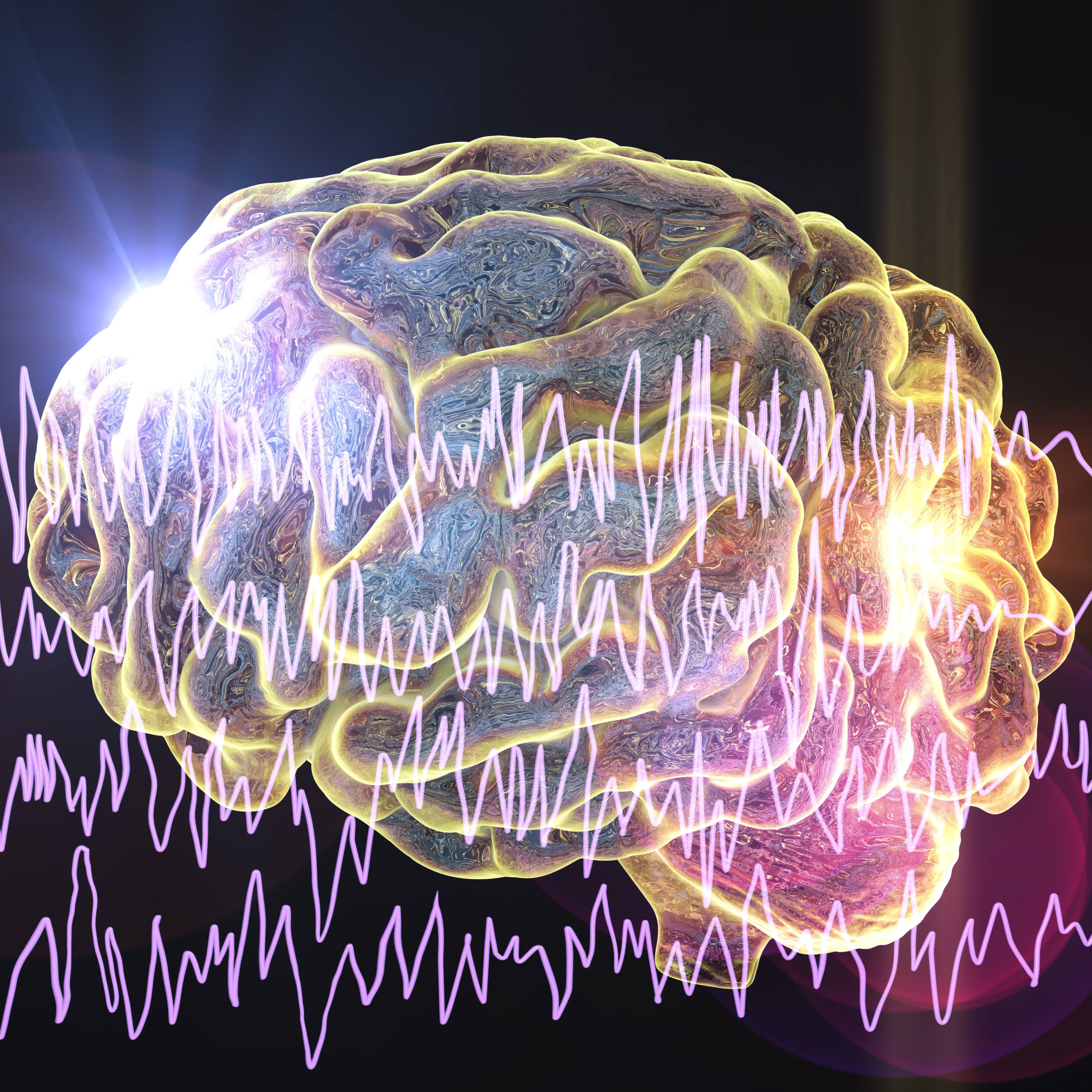
But some types of seafood — particularly large, predatory fish such as shark, swordfish, king mackerel and tilefish — can contain high levels of mercury. Although the mercury in seafood isn't a concern for most adults, special precautions apply if you're pregnant or planning to become pregnant. If you regularly eat fish high in mercury, the substance can accumulate in your bloodstream over time. Too much mercury in your bloodstream could damage your baby's developing brain and nervous system.
How much seafood is recommended?
The Food and Drug Administration, the Environmental Protection Agency and the 2015-2020 Dietary Guidelines for Americans recommend that pregnant women eat at least 8 ounces and up to 12 ounces (340 grams) of a variety of seafood lower in mercury a week. That's about two to three servings.
What's safe to eat?
Eat a variety of seafood that's low in mercury and high in omega-3 fatty acids, such as:
- Salmon
- Anchovies
- Herring
- Sardines
- Freshwater trout
- Pacific mackerel
Other safe choices include:
- Shrimp
- Pollock
- Tilapia
- Cod
- Catfish
- Canned light tuna
However, limit white (albacore) tuna and tuna steaks to 6 ounces (170 grams) a week.
Are there other guidelines for seafood during pregnancy?
Consider these precautions:
- Avoid large, predatory fish. To reduce your exposure to mercury, don't eat shark, swordfish, king mackerel or tilefish.
- Skip uncooked fish and shellfish. To avoid harmful bacteria or viruses, don't eat uncooked fish and shellfish, including oysters, sushi, sashimi and refrigerated uncooked seafood labeled nova style, lox, kippered, smoked or jerky.
- Understand local fish advisories. If you eat fish from local waters, pay attention to local advisories. If advice isn't available, limit fish from local waters to 6 ounces (170 grams) a week.
- Cook seafood properly. Most seafood should be cooked to an internal temperature of 145 Fahrenheit (63 Celsius). Fish is done when it separates into flakes and appears opaque throughout. Cook shrimp and lobster until the flesh is pearly and opaque. Cook clams, mussels and oysters until their shells open. Discard any that don't open.
Are there other ways to get omega-3 fatty acids?
Beyond seafood, other sources of omega-3 fatty acids include:
- Foods. Flaxseed — ground seeds or oil — canola oil, walnuts, sunflower seeds and soybeans (edamame) are all good sources of omega-3 fatty acids.
- Fortified foods. Yogurt, milk and eggs can be fortified with omega-3 fatty acids.
- Supplements. Supplements typically contain fish oil or omega-3 fatty acids from marine plant sources. Many prenatal vitamins also contain DHA. Talk to your doctor before taking any supplement.
Keep in mind that researchers haven't yet determined whether supplements can promote fetal brain development. While pregnant women can get omega-3 fatty acids from many sources, most experts recommend eating seafood for this purpose.
Though mercury can harm a developing baby's brain, eating average amounts of seafood containing low levels of mercury during pregnancy hasn't been shown to cause problems. And the omega-3 fatty acids in many types of fish can promote a baby's healthy cognitive development. As long as you avoid fish known to be high in mercury or contaminated with pollutants, seafood can be a regular part of your healthy-eating plan during pregnancy.
This article is written by Mayo Clinic staff. Find more health and medical information on mayoclinic.org.