-
Women’s Wellness: Lifestyle strategies ease some bladder control problems

If you've been struggling with the embarrassment and discomfort of a bladder control problem, you may be looking for ways to improve it. Fortunately, there are simple lifestyle changes that may improve bladder control or enhance response to medication.
Health care providers often call these strategies lifestyle modifications or behavior therapies. They're safe, easy, effective and inexpensive. You can try these techniques before trying other types of treatment, such as medications or surgery, or in combination with them.
Focus on fluids and food
How much fluid you drink can influence your bladder habits, and so might certain foods you eat.
Too much fluid
Drinking too much fluid makes you urinate more often. Drinking too much too quickly can overwhelm your bladder, creating a strong sense of urgency.
Even if you need to drink more because you exercise a lot or work outdoors you don't have to drink all fluids at once. Try drinking smaller amounts throughout the day, such as 16 ounces (473 milliliters) at each meal and 8 ounces (237 milliliters) between meals.
If you get up several times at night to urinate:
- Drink more of your fluids in the morning and afternoon rather than at night
- Skip alcohol and beverages with caffeine, such as coffee, tea and cola, which increase urine production
- Remember that fluids come not only from beverages, but also from foods such as soup
Too little fluid
Drinking too little fluid can lead to a buildup of body waste products in your urine. Highly concentrated urine is dark yellow and has a strong smell. It can irritate your bladder, increasing the urge and frequency with which you need to go.
Bladder irritants
Certain foods and beverages might irritate your bladder, including:
- Coffee, tea and carbonated drinks, even without caffeine
- Alcohol
- Certain acidic fruits — oranges, grapefruits, lemons and limes — and fruit juices
- Spicy foods
- Tomato-based products
- Carbonated drinks
- Chocolate
Consider avoiding these possible bladder irritants for about a week to see if your symptoms improve. Then gradually — every one to two days — add one back into your diet, noting any changes in urinary urgency, frequency or incontinence.
You might not have to eliminate your favorite foods and drinks entirely. Simply cutting down on the amount might help, too.
Try bladder training
When you have an overactive bladder, you can get used to urinating frequently or at the slightest urge. Sometimes, you might visit the toilet when you don't have the urge because you want to avoid an accident. After a while, your bladder begins sending "full" messages to your brain even when it's not full, and you feel like you have to urinate.
Bladder training, or retraining, involves adjusting your habits. You go to the toilet on a set schedule — even if you have no urge to urinate — gradually increasing the time between urination. This allows your bladder to fill more fully and gives you more control over the urge to urinate.
A bladder-training program usually follows these basic steps:
- Identify your pattern. For a few days, keep a diary in which you note every time you urinate. Your health care provider can use this diary to help you make a schedule for your bladder training.
- Extend your urination intervals. Using your bladder diary, determine the amount of time between urinating. Then extend that by 15 minutes. If you usually go every hour, try to extend that to an hour and 15 minutes. Gradually lengthen the time between trips to the toilet until you reach intervals of two to four hours. Be sure to increase your time limit slowly to give yourself the best chance for success.
- Stick to your schedule. Once you've established a schedule, do your best to stick to it. Urinate immediately after you wake up in the morning. Thereafter, if an urge arises, but it's not time for you to go, try to wait it out. Distract yourself or use relaxation techniques, such as deep breathing.If you feel you're going to have an accident, go to the toilet but then return to your schedule.
Don't be discouraged if you don't succeed the first few times. Keep practicing, and your ability to maintain control is likely to increase.
Strengthen your pelvic floor
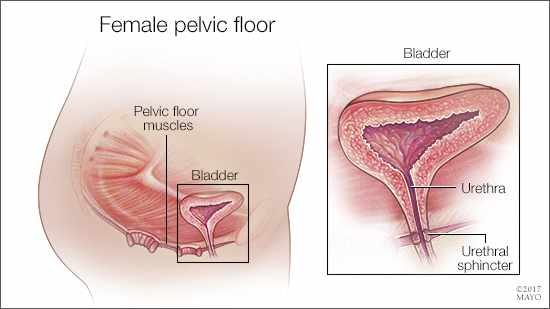
Your pelvic floor muscles and urinary sphincter help control urination. You can strengthen these muscles by regularly doing pelvic floor exercises, commonly referred to as Kegels.
The pelvic floor muscles open and close the tube that carries urine from the bladder to outside your body (urethra). These muscles also support the bladder during everyday activities such as walking, standing, lifting and sneezing.
- Practice Kegel exercises. To perform, squeeze your pelvic floor muscles — as if you're trying to stop your stream of urine — for three seconds. Relax for a count of three and repeat several times. Your doctor might recommend that you do a set of these exercises three or four times a day, lying down, sitting and standing.To be sure you're doing them correctly, ask your doctor or nurse to help you or to refer you to a physical therapist knowledgeable about pelvic floor exercises.
- Biofeedback. Biofeedback can help train pelvic floor muscles. Sensors placed near the muscles transmit exertion levels to a computer, which displays the levels on the screen. This immediate feedback may help you master Kegel exercises more quickly because you can see whether you're using the correct muscles. Biofeedback can be done with a professional or with a home device.
- Vaginal weights. Cone-shaped weights are another option used to help with Kegel exercises. You place a weight in your vagina and contract your pelvic floor muscles to keep it from falling out. Many cones come in sets of varying weights, so you can build up to heavier weights as your pelvic floor muscles strengthen.
Control contributing factors
Certain medications, excess weight, smoking and physical inactivity can contribute to bladder control problems. If you address these factors, bladder-specific techniques — such as avoiding bladder irritants and bladder training — might be more successful.
- Manage your medications. Drugs that might contribute to bladder control problems include high blood pressure drugs, heart medications, diuretics, muscle relaxants, antihistamines, sedatives and antidepressants. If you develop incontinence or difficulty urinating while taking these drugs, talk to your doctor.
- Maintain a healthy weight. Being overweight can contribute to bladder control problems, particularly stress incontinence. Excessive body weight puts pressure on your abdomen and bladder, sometimes resulting in leakage. Losing weight might help.
- Stop smoking. Smokers are more likely to have bladder control problems and to have more-severe symptoms. Heavy smokers also tend to develop a chronic cough, which can place added pressure on the bladder and aggravate urinary incontinence.
- Be active. Some studies indicate that regular physical activity improves bladder control. Try for at least 30 minutes of low-impact moderate activity — such as walking briskly, biking or swimming — most days of the week.
- Minimize constipation. Straining during bowel movements can damage the pelvic floor. Unfortunately, some medications used to treat bladder control problems can worsen constipation. Exercising, drinking enough water and eating high-fiber foods, such as lentils, beans, and fresh vegetables and fruit, might help improve constipation.
- Manage chronic cough. Your cough could be making your bladder problem worse. See your doctor about treatment options.
This article is written by Mayo Clinic staff. Find more health and medical information on mayoclinic.org.








