-
Cardiovascular
Mayo Clinic Q and A: Is it heartburn or a heart attack?
 DEAR MAYO CLINIC: My dad recently went to the emergency room with terrible chest pain and sweating, and was concerned he was having a heart attack. He was kept overnight for monitoring, but doctors said his heart was fine and that his symptoms were probably due to heartburn. Should I suggest he have more tests to determine if it’s something more serious? Are there things he can do to avoid having another episode like this?
DEAR MAYO CLINIC: My dad recently went to the emergency room with terrible chest pain and sweating, and was concerned he was having a heart attack. He was kept overnight for monitoring, but doctors said his heart was fine and that his symptoms were probably due to heartburn. Should I suggest he have more tests to determine if it’s something more serious? Are there things he can do to avoid having another episode like this?
ANSWER: In a situation like this, it’s important for your father to have a follow-up appointment with his primary care physician to confirm the underlying cause of his symptoms. The physician can do a more thorough evaluation, and refer him for more tests and a consultation with a cardiologist, if needed.
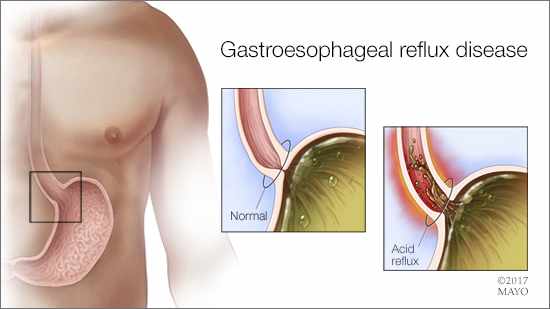
Heartburn, a burning sensation under the breastbone, is a symptom of gastroesophageal reflux disease, or GERD. It happens when stomach acid backs up into the esophagus — the tube that carries food from your mouth to your stomach. Although a burning sensation in the chest is common with GERD, its symptoms can vary widely. In some cases, GERD may feel like a dull ache or pressure in the chest, or, if it’s severe, GERD can lead to crushing chest pain. A heart attack, heart disease and other cardiac concerns can trigger similar symptoms.
Distinguishing the difference between the symptoms of GERD and those that could be related to a heart condition can be difficult. That’s because the nerves that lead to the heart and those that lead to the esophagus are located close to one another, so determining exactly where symptoms come from can be a challenge.
With that in mind, it’s important to confirm that chest pain is not heart-related. So, even if results of heart tests such as an electrocardiogram look fine in the emergency care setting, a more comprehensive evaluation still is needed. In many cases, that assessment includes a stress test to see how well the heart works during physical activity. Based on the severity of his symptoms and your father’s medical history, his physician can determine if he needs to see a cardiologist for additional testing.
It is possible that another condition unrelated to GERD or a heart condition could be causing your father’s symptoms, such as gallstones. In most cases, however, chest pain comes from a cardiac concern or GERD.
If the follow-up assessment shows that your father’s symptoms are due to GERD, there are a number of steps he can take to help prevent symptoms in the future. Overeating or eating a large meal and then lying down are the two most common heartburn triggers. Eating smaller meals and not eating two to three hours before going to bed often can reduce symptoms. Avoiding high-fat foods, spicy foods and citrus juices can be helpful, too. Many people who experience heartburn also find that reducing alcohol, caffeine and nicotine may decrease the frequency of symptoms.
Typically, GERD does not require treatment from a health care provider. Over-the-counter antacid medications are often enough to decrease symptoms, along with lifestyle changes. Some symptoms, however, should prompt a medical appointment, including food sticking in the esophagus, dark or bloody stools, unexplained weight loss or bouts of heartburn that happen more than two or three times a week.
The bottom line is that your father needs further evaluation to make sure he doesn’t have a heart condition. GERD can be managed, and nobody dies from it. But untreated heart problems can be fatal. It’s imperative your father have a formal cardiac evaluation at this time. — Dr. Jeffrey Alexander, Gastroenterology and Hepatology, Mayo Clinic, Rochester, Minnesota







