-
Featured News
Dementia-related pain: What caregivers need to know

Dementia isn't a specific disease. Instead, it describes a collection of symptoms that affect a person's thinking and social abilities enough to interfere with daily life. There are more than 55 million people worldwide living with dementia. Of these, 50% to 60% have Alzheimer's disease. Dementia is the seventh leading cause of death worldwide.
There is a constellation of dementia symptoms, and memory loss is the primary feature. Other common symptoms are physical functional decline and difficulty with mental tasks, like planning or spatial ability. Pain is another frequent symptom, although it is often overlooked and undertreated.
Dementia-related pain
As dementia progresses, so does the likelihood that patients are experiencing pain. Between 50% and 80% of patients with moderate to severe dementia experience pain daily. Many patients receive inadequate treatment due lack of recognition. Alzheimer's disease causes the person to develop a mask-like facial expression. This minimizes typical facial expressions of pain, like a drawn mouth or furrowed brows. Also, patients may have lost the cognitive ability to tell caregivers about their pain with phrases such as "this hurts" or "I am in pain."
Unfortunately, many patients with dementia are left with only basic expressions of pain presented through negative behaviors. These include screaming, cursing or striking out, particularly at caregivers.
Untreated pain also may cause patients to become more withdrawn or fatigued. This may be due to their discomfort or lack of solid sleep. Even though patients may feel drowsy and sleep more than before, their sleep is disturbed and not restorative. Patients may become more alert and interactive once their pain is treated, even if medications have a possible side effect of drowsiness.
Importantly, there is a marked increase in caregiver stress in those caring for patients experiencing pain.
Types of dementia-related pain
Chronic pain is pain that lasts longer than three months. It is associated with cognitive, emotional and social decline. The link between chronic pain and Alzheimer's disease is widely accepted despite not being fully understood.
Chronic pain affects some of the same areas of the brain that are affected by Alzheimer's disease. The changes occur in the area called locus coeruleus and affect a chemical messenger called norepinephrine. As this messenger is released, it causes the pain-relaying cells in the brain to become inflamed.
The degree of cognitive decline in a patient with Alzheimer's can be directly correlated with the severity of pain experienced. This means that a patient that does not have another apparent known cause of pain could still be experiencing significant pain. This is likely due to the neuroinflammation in the brain.
Other causes of pain include previous injuries and areas of surgery. Perhaps the patient had a knee or hip replacement or a tennis elbow injury when younger. These former injuries or conditions can become painful as patients become less mobile. Joints can become stiff and sore when not used regularly. The patient may avoid being repositioned or using painful body parts. This can contribute to developing contractures, which is the tightening of muscle, skin, tendons and tissues. Pressure ulcers can develop from spending a significant amount of time in the same position and lead to pain.
Other medical conditions, like cancer, heart disease or kidney disease, can cause pain. These types of pain can be more difficult to assess. Caregivers may not realize the disease has worsened because patients cannot verbally express how they are feeling. Swelling or other symptoms may not be easily noticed if the person is bedridden. And patients have a hard time expressing nuanced symptoms like chest or flank pain.
Finally, mental pain can be exasperated by dementia. Patients may experience significant loss or grief, even when confused or disoriented. This can lead to social, spiritual or emotional pain, which is felt physically like other types of pain.
Assessing pain
Patients often are asked to rate their pain on a scale of 1 to 10. This isn't an option for patients with moderate to severe dementia. They're not able to verbally express or rate their pain or discomfort.
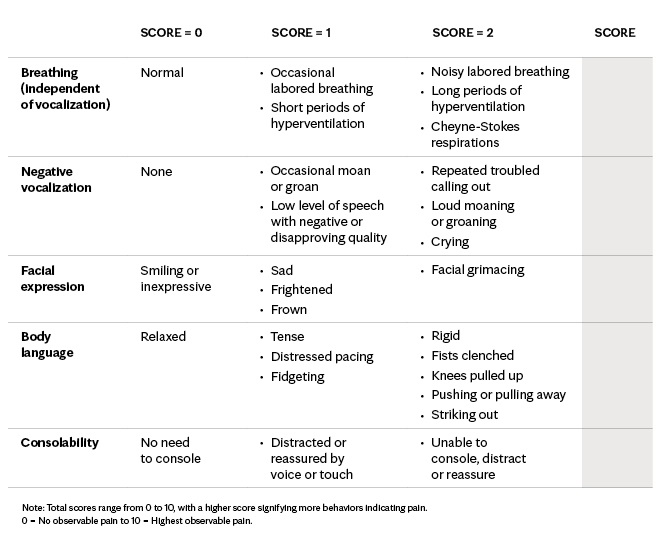
The Pain Assessment in Advanced Dementia Scale (PAINAD) was developed to assess pain and reduce the likelihood that it is unrecognized and untreated. It's easy to learn and use by people without prior medical training and does not require the patient to have language skills.
Medication treatment
When treating pain, health care teams always want to prescribe the lowest dose of medication. Narrowing in on the type of pain that a patient is experiencing helps achieve this goal. For example, a patient likely has neuropathic pain if the pain burns, tingles or travels from one area to another. This requires medications that are specific to the nervous system. Other medications are used to treat inflammation.
Some pain is caused by many things, such as cancer pain. This may require several medications, each with a specific role. When used together, lower doses of each medication may be all that is necessary to ease the pain. This is referred to as multimodal pain therapy.
Nonmedication treatment
Sometimes, pain medication is not necessary, and patients can get pain relief through other treatments.
Massage can be beneficial and ease the pain. A caregiver doesn't need to be a trained massage therapist to help. If you know that your grandmother had a knee replacement and her knee feels warm or swollen, gently massage it and gauge her reaction. She may not be able to tell you that it feels good, so watch if her body position and facial expression relax and her breathing slows. These physical cues will help you know that what you are doing is helpful.
Music therapy is a beautiful approach to pain management. You don't need to be a trained music therapist, as just knowing what grandpa liked to listen to in his youth can help. Playing music can distract him temporarily and release natural endorphins to reduce pain. Music also can help orient patients and bring pleasant feelings and memories.
Other treatments could include aromatherapy, a visit from a pet therapy animal or drawing with your loved one. Families can do these activities together with no additional training needed.
Finally, don't underestimate the power of repositioning. If your loved one looks uncomfortable, gently shift him or her into a new position. Watch for relaxed facial expressions or body language to ensure the new position feels better. Frequent position changes enhance comfort and improve blood flow to the skin, which protects against pressure sores.
Caregiver tips
Caregivers play an important role in assessing pain and advocating for treatment.
Understand how to assess signs or symptoms of pain using the PAINAD scale and follow the ALTAR acronym to address potential pain in your loved one with dementia:
- Anticipate
Expect that your loved one with dementia will experience pain at some point. Be proactive early in the disease process to help ensure pain is not left untreated. Familiarize yourself with the PAINAD scale. Be prepared to advocate for your loved one through caregiver education and physician visits. Review advocacy tips. - Look
Watch for common causes of pain. Look, touch, listen and think about the different types of pain your loved one may be experiencing. Inspect your loved one's mouth for oral sores due to decay or ill-fitting dentures. Inspect feet for skin lesions or issues from ingrown toenails. Do you see your loved one wince or guard against gentle pressing on the abdomen? Feel large joints, like knees and hands. Do they feel warm or is one swollen? Does your loved one appear more comfortable in certain positions? - Treat
Review nonmedication treatment options and incorporate these into your care. Bring music from their youth, massage sore joints or color together. Talk with the health care team about any concerns and if medications are necessary. - Avoid comparisons
It's easy to compare your loved ones today to past selves. This is not helpful and should be avoided. People with dementia don't process pain in the same way they did before their diagnoses. Your loved one may have bragged about having a high pain tolerance in the past but is experiencing pain differently now. Medications and other treatments may be necessary. - Revisit
Treatments that worked last week may not work today. A few "good days" does not mean the pain is under control over the long term. Consistently revisit the types of pain, treatments, positioning, time of day and other factors affecting your loved one's pain.
Advocacy tips
Caregivers play an important role in advocating for their loved ones' pain management, especially if they cannot advocate for themselves.
Follow these tips when navigating appointments, hospital stays and long-term care needs:
- Attend all appointments or hospital rounds.
- Write down questions and topics you want to discuss with the care team.
- For sensitive topics, send questions to the care team before the appointment or ask to speak in private.
- Ask about the different types of pain and explain previous injuries or chronic conditions that could contribute to pain levels.
- Document your loved one's baseline functionality and the changes you witness.
- Document pain levels often and note the time of day, position, mood, etc.
- Make sure your loved one wears needed eyeglasses, dentures, hearing aids or other assisted devices.
- Bring comfort items, like your loved one's favorite blanket, to appointments.
Most patients with moderate to severe dementia, including Alzheimer's disease, experience pain. Work with your loved one's care team to get the pain under control. This will increase comfort and peace of mind while decreasing outbursts, aggression, withdrawal and delirium.
Jennifer Winegarden, D.O., is a physician in Palliative Care in La Crosse, Wisconsin.







