-
Mayo Clinic Q&A podcast: Imaging plays key role in improving endometriosis treatment
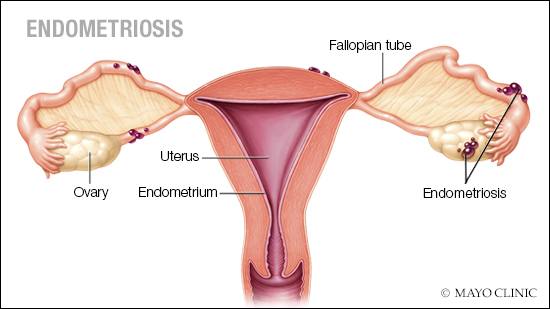
Endometriosis is often a painful disorder in which tissue similar to the tissue that normally lines the inside of the uterus — the endometrium — grows outside the uterus.
"Endometriosis is a very common condition," explains Dr. Tatnai Burnett, a gynecologic surgeon at Mayo Clinic. "Most of our studies, which are looking at women who have symptoms, would suggest that about 1 in 10 women, so 10% or so have endometriosis. Now, the difficulty here is that some women do not have significant symptoms and wouldn't go to a doctor, or they minimize their symptoms or think what they are experiencing is normal. So, if anything, that estimate is probably on the low side of what actual reality is."
With endometriosis, the endometrial-like tissue acts as endometrial tissue would — it thickens, breaks down and bleeds with each menstrual cycle. But because this tissue has no way to exit the body, it becomes trapped. Endometriosis can cause pain, which is sometimes severe, especially during menstrual periods. Fortunately, effective treatments are available.
The role of imaging
Imaging, including ultrasound and MRI, is an important step in evaluating patients with endometriosis and can impact treatment options and surgical planning.
"Ultrasound is a great way to start the evaluation of the female pelvis because it's easily accessible," says Dr. Wendaline VanBuren, a Mayo Clinic radiologist who specializes in gynecologic imaging. "And it gives us a lot of information about the ovaries and the uterus. The problem with endometriosis is that, while it can involve the ovaries, it can involve all these sites on the surface of the uterus, the bowel, the ureters and all the structures around it. So, MRI gives us a little bit more of a global perspective of the pelvis. So that's the advantage of using MRI."
To better coordinate care for patients with endometriosis, Drs. Burnett and VanBuren instituted an MRI-based interdisciplinary conference at Mayo Clinic that brings together radiology and gynecology.
"For endometriosis, we realized that a multidisciplinary approach where we review things together was just in the best interest of the patient because it gives us the best coordination of care between the radiologist and the gynecologist," says Dr. Burnett. "It gives us a nuanced interpretation of what the imaging means for the patient. And then it allows us to apply what we see in the imaging to our surgical plan and to the surgical team. We use all the information that we gather to really make the best plan for the patient in regard to the patient's goals and what they need."
The team at Mayo Clinic has been sharing the success of this collaborative model and educating other experts through the publication of their research findings and participation in a disease-focused endometriosis panel through the Society for Abdominal Radiology.
"We all have our own expertise," says Dr. VanBuren. "And when we're able to collaborate and share, hearing the clinical stories, looking at the imaging, putting it together, the considerations for management, whether that be medical or surgical planning, we're really able to make a huge impact. It's exciting to see now collaborations between societies, from gynecology and radiology together."
On the Mayo Clinic Q&A podcast, Drs. Burnett and VanBuren discuss the multidisciplinary approach to diagnosing and treating endometriosis.
Watch: Dr. VanBuren and Dr. Burnett discuss imaging and treatment for endometriosis.
For the safety of its patients, staff and visitors, Mayo Clinic has strict masking policies in place. Anyone shown without a mask was either recorded prior to COVID-19 or recorded in a nonpatient care area where social distancing and other safety protocols were followed.







