There is new hope in the fight against glioblastoma, the deadliest and most aggressive form of primary brain cancer.
Currently there is no cure, but results of a new study conducted at Mayo Clinic show patients experienced improved overall survival while maintaining quality of life after undergoing a novel approach to treatment.
Watch: Breakthrough in the fight against glioblastoma
Journalists: Broadcast-quality video (2:45) is in the downloads at the end of this post. Please courtesy: "Mayo Clinic News Network." Read the script.
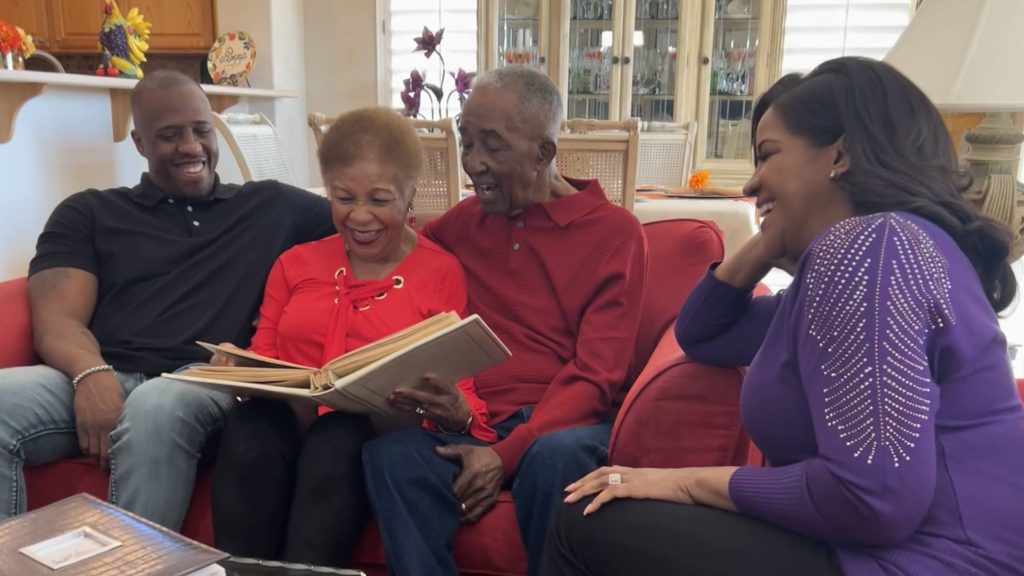
Richard Casper was one of the study participants. The Arizona man enrolled in the clinical trial at Mayo Clinic in Phoenix after his diagnosis of glioblastoma in 2019. Richard was given only months to live, but his family says thanks to his strength, perseverance, and innovative medical care, he survived nearly double the amount of time.
"To be almost two and a half, three years in after being told you only have a few months, it's quite remarkable," says Susan Casper, Richard's daughter.
Richard succumbed to the disease in 2023. During the treatment, his family says he had little to no side effects. In the months before his passing, Richard stated, "I feel great. If someone didn't tell me I have the glioblastoma, I wouldn't even know it."

The clinical trial was led by Dr. Sujay Vora, a radiation oncologist at Mayo Clinic in Arizona. The small, single-arm study incorporated the use of advanced imaging technology combined with cutting-edge radiation therapy in patients over the age of 65 with newly diagnosed World Health Organization (WHO) grade 4 malignant glioblastoma.
"The patients lived longer than we expected. This patient population is expected to live six to nine months. Our average survival was 13.1 months. There were some patients that were out closer to two years. The results exceeded our expectations. We are very pleased," says Dr. Vora.
The study is published in The Lancet Oncology.

Why is glioblastoma so deadly?
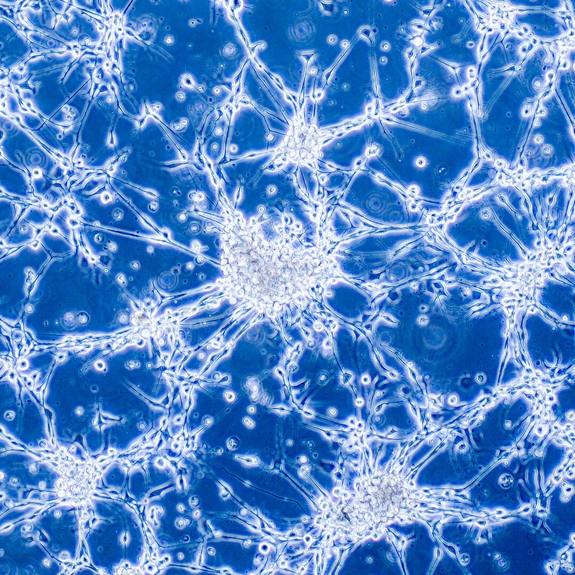
Glioblastoma is among the most challenging cancers to treat. The disease is aggressive and invades healthy brain tissue with hairlike tentacles. "That is why doing a complete surgery is very difficult, as compared to say breast cancer, where a lumpectomy can be performed to remove not only the tumor, but a healthy rim of tissue around it," explains Dr. Vora.
Surgery for glioblastoma presents a different set of obstacles. "When it comes to glioblastoma, it is challenging to do that level of surgery. You try to surgically remove whatever you can safely without leaving the patient worse off after surgery."
Another factor that makes glioblastoma so lethal is that it can be fast- growing and unresponsive to treatment.
"These cancer cells are quite challenging to overcome," says Dr. Vora. "There are some patients we see after their surgery, and by the time we are ready to start their treatment, they've already had a recurrence of the disease."
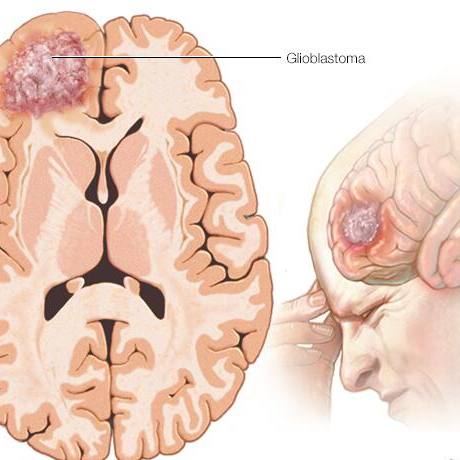
An estimated 14,500 people will be diagnosed with glioblastoma in the U.S this year. "In the best of circumstances the average survival rates are in the 14-15 month range. But for patients 65 and older, the group that was the focus of our study, patients do even worse. The prognosis for this population is between six and nine months," says Dr. Vora.
Symptoms of glioblastoma
- Headache
- Nausea and vomiting
- Confusion or decline in brain function
- Memory loss
- Personality changes
- Vision changes
- Speech difficulties
- Trouble with balance
- Muscle weakness
- Seizures
Attacking glioblastoma with a triad
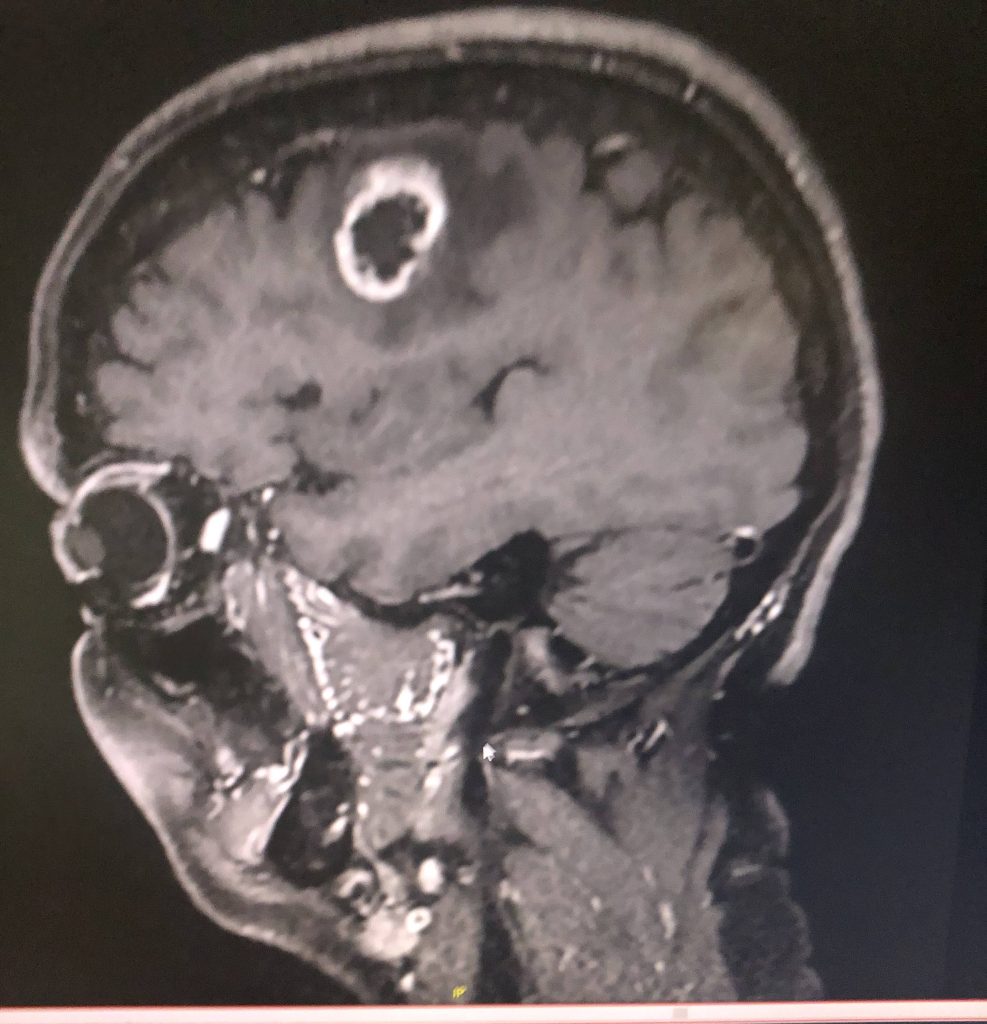
For the clinical trial, Dr. Vora and his team mapped out a plan that would allow them to be more intentional and precise with treating the location of the glioblastoma.
"It is the triad of metabolic imaging, proton beam therapy and hypofractionation, which is a shorter course of radiation that might be the best combination to treat glioblastoma in the 65-and-older patient population."
Dr. Sujay Vora, radiation oncologist & Principal study investigator
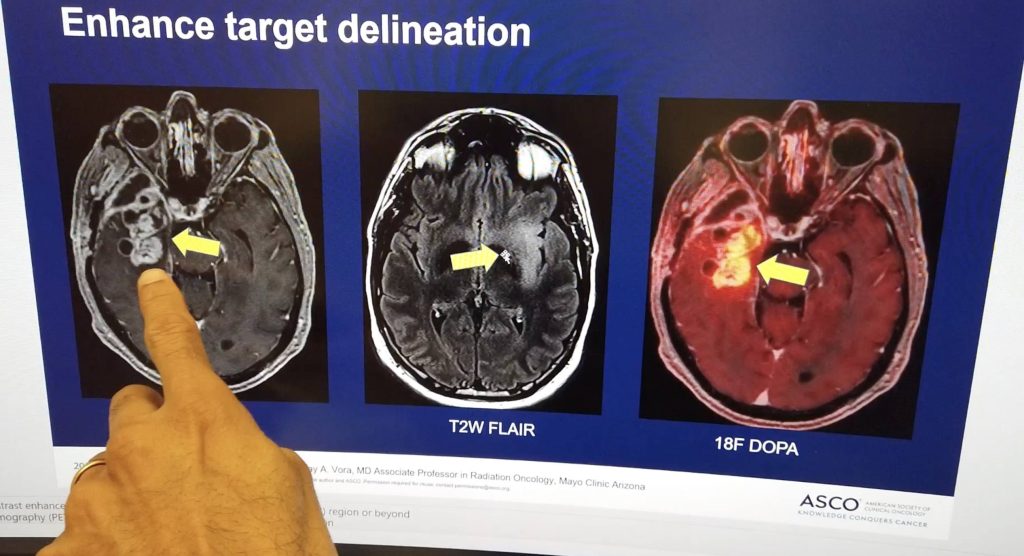
The imaging incorporated the use of 18F-DOPA PET and contrast-enhanced MRI. "18F-DOPA PET is an amino acid tracer that can cross the blood brain barrier, and it can accumulate within the glioblastoma cells itself," says Dr. Vora.
Researchers combined these images to determine the location of the most metabolically active "hot spots" of the cancer in the brain.
Taking aim with proton beam therapy
Study investigators used one of the most advanced forms of radiation treatment, called proton beam therapy.
"With standard radiation, the beams go through the brain tissue, so there's an entrance dose and the exit dose. But with proton beam therapy, we dial up how deeply we want the radiation to go," explains Dr. Vora. "It drops off its energy in the tumor, and then there's basically no radiation after that. It allows us to be more preferential into the delivery of radiation and protect more of the healthy surrounding tissue."
During proton beam therapy, a patient lies on a table while the machine rotates around the patient's head targeting the tumor with an invisible beam. The patient is awake for the procedure. It is painless with many patients reporting fewer to no side effects.
Unlike traditional radiation for glioblastoma, which is typically delivered over the course of three to six weeks, treatment with proton beam therapy for the study was conducted in one to two weeks.

"I am hopeful that this is the first step of many where we can continue to move the needle and allow patients to live longer and live well," says Dr. Vora. "The goal is to improve the outcomes for our patients allowing them to spend more time with their families."
Nadya's story
2022 was a tough year for Nadya El-Afandi. She was on the verge of celebrating a long but successful battle with breast cancer.
"Out of the blue, I had a seizure. I went to the hospital, they did an MRI. After additional tests they told me the news: 'You have a glioblastoma,'" recalls Nadya. She asked her doctor if she should continue her breast cancer treatment. "He said, 'No'-meaning the glioblastoma would kill me before the breast cancer."
Nadya was not about to give up.

Nadya is a wife and mother of four children. She lives just outside of Rochester, Minnesota. "My children said to me, 'Mom, you're a unicorn. Of course you'll live.' My mother has had a number of medical conditions and we never expected her to live this long. And she's still alive and with us," says Nadya. "My children have also said, 'You've got grandma's blood in you. You will live.'"
Nadya is receiving care at Mayo Clinic in Rochester. That's where she learned about a new clinical trial called SAGA, or stereotactic ablative radiation treatment for glioblastoma. The phase 2 clinical trial is building upon Dr. Vora's research and studying a larger group of patients. The study is being led by Dr. William Breen, radiation oncologist at Mayo Clinic in Rochester.
Our goal is to transform the way we treat glioblastoma - in that we are using advanced imaging to help us better target the tumor. We're looking at shorter courses of radiation to minimize the burden on patients and their families and hopefully complete effective and safe treatment in a shorter amount of time.
William Breen, M.D., Radiation Oncologist
It has been 15 months since Nadya began treatment for glioblastoma. So far, there is no sign the glioblastoma has returned. "Nadya has already exceeded the time that's expected time to have a tumor recurrence, and she continues to do well," says Dr. Breen. "Nadya is beyond some measures of what the average, overall survival time would be."
While Nadya's progress in encouraging, Dr. Breen says it is important to note that it is too early to draw any conclusions about safety or efficacy of this approach to treatment until the study is completed.
Meanwhile, Nadya is focused on living her life to the fullest. Fifteen months after undergoing treatment, Nadya embarked on an adventure to Hawaii, where she spent time taking helicopter tours, snorkeling and hiking.
"We are living on the edge of medical miracles, and we are riding that tide. There's no cure for glioblastoma yet. But I've been able to take advantage of this medical opportunity, and it has given me a quality of life that is just outstanding. Every day is the best day and I'm going to enjoy every minute of it."
Nadya El-Afandi, glioblastoma patient

photo courtesy: Nadya El-Afandi
Related articles
- Breakthrough in treatment approach showing promise in the fight against glioblastoma, the deadliest and most aggressive type of brain cancer
- (VIDEO) Focus on hope: Brescia’s Story
- All-Star pitcher Liam Hendriks shares how he closed out cancer at Mayo Clinic in Arizona
- Cancer is tough. Evelyn Owens is tougher
- https://cancerblog.mayoclinic.org/2021/12/21/glioblastoma-in-older-adults-improving-survival-and-quality-of-life/
- https://cancerblog.mayoclinic.org/2024/05/15/technology-clinical-trials-offer-hope-after-glioma-diagnosis/